Deep Brain Stimulation (DBS) is a therapy used to manage movement disorders and other brain conditions. In children, DBS is used mainly for dystonia, a movement disorder which involves ‘too much’ movement, causing twisting and/or abnormal postures that is out of the person’s control. DBS involves implanting a device which sends electrical signals to the movement centre within the brain (the part of the brain responsible for all movements and motion of the body), to change the brain messages causing dystonia.
Who is suitable for DBS?
DBS may be suggested as a treatment for your child if they have:
- a confirmed or suspected genetic cause of dystonia, without injury to the brain seen on imaging, and/or
- severe dystonia that is impacting your child’s life despite medical and other supportive therapies (e.g. positioning or avoiding triggers).
What does DBS involve?
- DBS involves a surgery where thin wires (electrodes) are placed inside the brain and connected to a battery that is placed under the skin on the upper chest (like a heart pacemaker) or tummy.
- The thin wires (electrodes) travel under the skin down into the middle of the brain where the movement centre of the body is located.
- These wires send a continuous electrical signal to stimulate the deep brain areas controlling voluntary movements.
- The battery is programmed to deliver therapy tailored to your child’s symptoms.
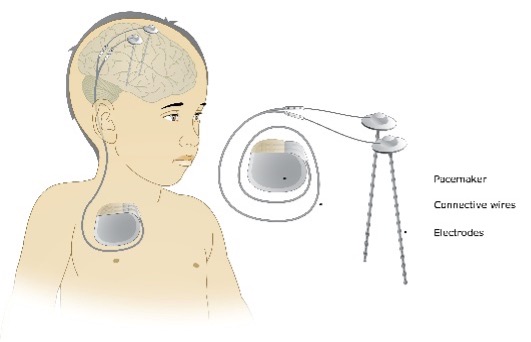
Figure 1: Deep Brain Stimulation device
What to expect with DBS surgery?
Before DBS surgery
Your child will have an
MRI scan up to three months before surgery. This is used to plan exactly where to place the DBS wires. This is usually done under general anaesthetic to make sure your child does not move
Do not give your child ibuprofen, aspirin, other non-steroidal anti-inflammatory medications (e.g. nurofen) or fish oil supplements for two weeks before surgery. These medications can increase the risk of bleeding throughout the surgery. It is safe to have paracetamol at any time.
Some other non-prescription items can also increase bleeding risk during the procedure. Please discuss all the medicines and vitamins that your child takes with your child’s surgeon or clinical nurse consultant.
You will also be notified of your child’s fasting times before the surgery.
During DBS surgery
Your child will be admitted to hospital on the day of surgery. Your child’s hair will be partially shaved for the surgery but will grow back over time following the surgery.
The surgery is performed by senior neurosurgeons experienced with DBS, with a specialised team of anaesthetists and nurses. Neurologists are also present to help ensure the DBS electrodes (wires) are in the correct place.
The surgery is performed with your child asleep under general anaesthetic for the entire procedure, and generally takes between four to six hours to complete. The surgery occurs in two parts:
- During the first part of surgery, DBS wires are placed into the movement centre of the brain using a specialised GPS system.
- Your child will then have a CT scan. The CT images are combined with the MRI scans taken before surgery, creating a digital model of the brain. Using this model, the exact location to place the DBS wire is finalised.
- A small hole is drilled through the skull on one side and a tiny test wire is passed into the brain, towards the planned DBS target.
- Brain signal recordings are used to check the wire is in the correct spot.
- The test wire is then replaced by a permanent DBS wire. This procedure is repeated on the other side of the brain.
- The second part of the surgery involves placing the extension wires and the battery device under the skin, which are then connected to the DBS electrodes. The extension wires usually pass behind the ear and down the neck towards the battery device. This is usually placed over the left side of the upper chest. All parts of the DBS system are under the skin.
- Your child will have several scars following surgery such as on the top of the head, behind the ear, and on the upper chest where the battery is placed. Dissolvable stitches are used to close the wounds.
After DBS surgery
Your child will be required to stay in hospital for about a week so they can recover and their wounds can heal. There can be pain and bruising over the neck area and over the battery device in the first few days.
Your child will receive antibiotics via a drip, pain medication and anti-nausea medications to reduce the risk of infection of the wounds and for any pain they may feel.
In the days after surgery, your child will have a CT scan to check the DBS system is intact and in the correct location.
Your child will be seen by a physiotherapist before going home to ensure they are getting out of bed and moving around safely.
Your child’s neurologist will switch on the DBS therapy before your child goes home. This will usually be at a low setting, and allows your child to get used to living with DBS. Further adjustments will be made at regular appointments.
In the first few days after surgery, your child’s dystonia may be worse, better or unchanged. This does not predict how deep brain stimulation will help your child’s dystonia in the long term. It can take months to years for the continuous electrical signals to reduce dystonia. Most of the benefit can be seen in the first 12 months after surgery. This varies for individual children depending on the cause of their dystonia.
Care at home
Your child will have dissolvable stitches following surgery. You will be given instructions on how to care for these before you go home.
The DBS system must be checked daily and charged multiple times a week. You will be shown how to do this before you go home. If you are having problems charging the DBS at home, or you are concerned about DBS therapy, please contact your child’s treating team.
If you are worried about your child’s surgical wounds (such as leaking fluid, or if they look red and inflamed), please contact your child’s treating team.
Follow-up
Before going home, follow up appointments will be made with your child’s neurologist. They will initially be seen monthly following surgery for DBS therapy adjustments. They will also have routine allied health and medical assessments at three, six, nine and 12 months following surgery. These appointments are important to check on your child’s recovery and to tailor DBS therapy to your child. If DBS is working well, your neurologist may consider a reduction in your child’s usual medications over time.
Please note, you must tell the doctors that your child has DBS every time they are in hospital for any reason as special precautions may need to take place.
Key points to remember
- DBS is a therapy involving electrical stimulation to the brain to change the abnormal signals causing a movement disorder or another brain condition.
- It involves a neurosurgical operation where wires are placed deep into the brain and a battery is placed under the skin, usually on the upper chest.
- The DBS system must be checked daily and charged multiple times a week for stimulation therapy to continue.
- Deep brain stimulation is a treatment option for children with severe dystonia.
- Dystonia is a movement disorder which involves ‘too much’ movement, causing twisting and/or abnormal postures, that is out of the child’s control.
- Benefit from DBS takes time as therapy is increased gradually. You will not see its effects straight after surgery. Most of the benefit occurs over the 12 months after DBS has started however, you can continue to see improvement after this time.
- You must tell the doctors that your child has DBS every time they are in hospital for any reason.
For more information
Common questions our doctors are asked
Is DBS implanted under the skin?
Yes, a rechargeable battery is placed under the skin on the upper chest or tummy which is connected to wires extending into the middle of the brain, which are also placed under the skin. No parts of the DBS system are outside the skin.
Does DBS require an operation?
Yes, DBS involves a neurosurgical operation to place the DBS system inside the body. Your child will be asleep for the surgery and will be required to stay in hospital for approximately a week.
When will my child see results of DBS therapy?
It can take months to years for the continuous electrical signals to reduce dystonia. Most of the benefit can be seen in the first 12 months after surgery. This varies for individual children depending on the cause of their dystonia.
DBS can help dystonia but cannot treat spasticity (uncontrolled muscle stiffness and tightening). DBS does not improve intellectual function. Improvements in mood and interaction with medication reduction are sometimes seen after DBS therapy is started. Your child’s treating team will discuss he potential benefits and the limitations of DBS therapy with you.
Developed by The Royal Children's Neurology and Neurosurgery departments. We acknowledge the input of RCH consumers and carers.
Developed July 2021.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.