| Condition |
Management |
|
Neonatal conjunctivitis
Pathogens include staphylococcus, haemophilus, streptococcus, chlamydia, gonococcus and herpes simplex
Consider gonococcal conjunctivitis if severe purulent discharge with conjunctival and lid oedema

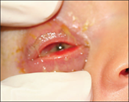
Gonococcal ophthalmia neonatorum with swelling, purulent discharge, injection of the conjunctiva and chemosis |
- Obtain conjunctival swabs for gram stain, giemsa stain and cultures, and gonococcal and chlamydia PCR if clinical suspicion
- Gonococcus, chlamydia and herpes simplex can cause invasive disease and may require septic work up. Seek specialist advice (eg neonatology, infectious diseases, general paediatrics, ophthalmology). See Recognition of the seriously unwell neonate
- Treat chlamydial conjunctivitis with oral azithromycin 20mg/kg once daily for 3 days and eye toilet
- Treat gonococcal conjunctivitis with a stat dose of ceftriaxone 25-50mg/kg. Where possible, ceftriaxone should be avoided in neonates
<41 weeks gestation, particularly if jaundiced or receiving calcium containing solutions. See Antimicrobial guidelines
- Herpes simplex infection and/or keratitis is likely to require septic work up and treatment with IV aciclovir. Seek specialist advice
- Treat other organisms with topical chloramphenicol 0.5% eye drops 4–6 times per day for 5–7 days
|
|
Subconjunctival haemorrhage
Painless and no discharge
Associated with activities that increase intraocular pressure; coughing, sneezing, vomiting, valsalva, strangulation
Potential sign of penetrating eye injuryif history of trauma. If the posterior extent of the haemorrhage cannot be visualised consider an orbital or base of skull fracture
- In infants, subconjunctival haemorrhage may be a sign of non-accidental injury

Extensive bilateral subconjunctival haemorrhages from excessive vomiting

Subconjunctival haemorrhage of temporal bulbar conjunctiva
|
- Observe. If isolated, usually resolves spontaneously within 1 – 3 weeks
- If recurrent, investigate cause (eg bleeding disorder). Consider non-accidental injury
|
|
Foreign body
Presents with watery discharge and/or sensation of foreign body
Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240. Available at https://www1.racgp.org.au/ajgp/2020/december/acute-red-eye-in-children |
See
Acute eye injury |
|
Corneal abrasion
Presents with watery discharge and pain that is normally severe initially and then subsides over 24 – 48 hours
 
Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240. Available at https://www1.racgp.org.au/ajgp/2020/december/acute-red-eye-in-children |
See
Acute eye injury |
|
Chemical/thermal burns
Presents with pain, watery discharge, conjunctival inflammation or pallor in more severe burns and/or corneal epithelial defect and/or corneal opacity
Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240. Available at https://www1.racgp.org.au/ajgp/2020/december/acute-red-eye-in-children |
- See
Acute eye injury
- Requires urgent, copious irrigation, after local anaesthetic. Sedation or urgent GA may be required
|
|
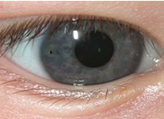
Infectious keratitis
Presents with purulent discharge, severe pain, vision loss, intense inflammation of the conjunctiva and corneal opacity (round white spot), or ulcer (dendritic in herpes and varicella) visible after fluorescein staining
Can be caused by bacteria, viruses, or fungi
Often associated with contact lens wear
Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240. Available at https://www1.racgp.org.au/ajgp/2020/december/acute-red-eye-in-children |
- Contact ophthalmology urgently
- Keep contact lens if possible for culture
|
|
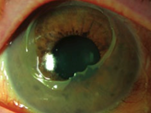
Endophthalmitis
Presents with severe pain, purulent discharge, vision loss, intense inflammation of conjunctiva and hypopyon
Risk factors: recent eye surgery, penetrating eye injury, keratitis

Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240. Available at https://www1.racgp.org.au/ajgp/2020/december/acute-red-eye-in-children |
- Contact ophthalmology urgently
- Likely to require broad spectrum IV antibiotics:
ceftazidime 50mg/kg (maximum 2g) 8 hourly
and
vancomycin 15mg/kg (maximum 750mg) 6 hourly |
|
Episcleritis and scleritis
Episcleritis presents with eye irritation/mild ocular tenderness, sectoral congestion of episcleral vessels and lacrimation
Scleritis presents with watery discharge, severe pain, vision loss and intense inflammation of sclera, episcleral and conjunctiva
Both associated with systemic inflammatory disease |
- Contact ophthalmology (urgent for scleritis)
- Consider systemic inflammatory disease/autoimmune disease
|
|
Iritis/Uveitis
Inflammation of the iris (iritis), ciliary body (cyclitis), or choroid (choroiditis)
Presents with pain, photophobia, blepharospasm and lacrimation
Pupil may be small, irregular and poorly reactive
Causes are autoimmune, infection, and trauma |
Contact ophthalmology |
|
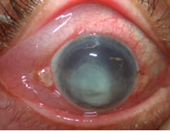
Acute angle closure glaucoma
Presents with severe eye pain, watery discharge, decreased visual acuity (cloudy vision), cloudy cornea and fixed mildly dilated pupil
May also have associated headache and vomiting (from raised pressure) |
Contact ophthalmology urgently |