See also
Penetrating eye injury
Eye examination
Acute red eye
Key points
- Consider a serious eye injury when a child presents with a painful eye or blurred vision
- Adequate analgesia will aid examination and procedural sedation may be required in the younger child
- Seek senior clinician or ophthalmology assistance early if eye assessment is proving difficult in the distressed child
- Chemical burns, especially alkali, need immediate irrigation
- If a penetrating eye injury is identified or suspected, stop examination, place an eye shield over the eye, keep nil by mouth and urgently refer to ophthalmology, see
Penetrating eye injury
Background
- Paediatric eye injury is common, and it is important to differentiate minor trauma from sight threatening conditions
- Sharp instruments are the most common cause of injury, followed by plants, animals, toys, or sports related injury
The following traumatic conditions threaten vision:
- Ruptured globe
- Retrobulbar haematoma
- Foreign body, either intraocular or corneal
- Large hyphaemas (causing acute glaucoma)
- Retinal detachment
- Corneal burns, either chemical or thermal
- alkalis penetrate deeper and have greater potential for serious injury and delayed burns
- Contact lens-related corneal infections (bacterial keratitis), see
Acute red eye
Assessment
The principles of eye trauma evaluation include:
- Manage other life-threatening injuries, see
Primary survey
- Ensure structural integrity of the globe
- Assess vision in the injured and uninjured eye
- Seek ophthalmology assessment where necessary
History
When assessing the injured and painful eye, the following questions should be asked:
- Proximity to chemicals or high velocity projectiles (particularly air guns, lawn mowers, power tools, hammering or motor vehicle accidents)
- Prolonged contact lens use
- Pain, foreign body sensation, tearing or photophobia
- Visual disturbance either temporary or persisting, including flashes or floaters in vision
- Eye discharge
- First aid provided
Eye examination
- See Eye Examination for full eye examination
- Adequate analgesia will aid assessment and procedural sedation may be required in the younger child
- Topical anaesthetic such as tetracaine (amethocaine) 0.5% or 1% can be used to assist with examination
- One drop into the affected eye will induce anaesthesia after 20 seconds and the effect lasts 10 – 20 minutes (longer with 1%)
- Avoid repeated administration of anaesthetic eye drops due to direct epithelial toxicity that can delay corneal healing
Globe
For obvious penetrating eye injuries or ruptured globe see
Penetrating eye injury
Assess for globe rupture or laceration:
- Severe loss of vision or loss of red reflex
- Loss of ocular motility
- Asymmetric, irregular pupil
- Hyphaema
- Distorted appearance of globe
- Localised conjunctival haemorrhage or chemosis (bulging of the conjunctiva)
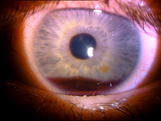
Hyphaema after blunt trauma
Management
Assessment and management of eye trauma should occur after management of other life-threatening injuries and consideration of head and C-spine injury
Penetrating eye injury
If a penetrating eye injury is identified or suspected, stop examination, place an eye shield over the eye, keep nil by mouth and urgently refer to ophthalmology, see
Penetrating eye injury
Retrobulbar haematoma
- Occurs due to blunt trauma leading to compartment syndrome and optic nerve compression
- Tense proptosis, limited eye movements, decreased visual acuity and Relative Afferent Pupillary Defect (RAPD)
- Emergent ophthalmology referral, may require urgent decompression

Left retrobulbar haematoma
Orbital blow out fracture
- Occurs due to high energy blunt trauma that increases intra-orbital pressure
- Symptoms include pain and diplopia (particularly on upward gaze), tenderness, eyelid swelling, nausea, and vomiting
- Signs can include ptosis, tenderness, relative enophthalmos, decreased sensation of cheek, lower eye lid crepitus
- CT of the orbit and ophthalmology referral

A 4yo child with right orbital blow out fracture associated with entrapment
Corneal abrasions and foreign bodies
- Seek ophthalmology advice and removal of:
- Embedded or metallic foreign bodies and avoid removing
- Large, deep, or central corneal foreign bodies
- If large (>2mm) or deep defect seen, presume full thickness abrasion and manage as per
penetrating eye injury
- Anaesthetise conjunctiva with one drop tetracaine (amethocaine) 1% or oxybuprocaine (benoxinate) 0.4%
- Examine surface of eye and under lids by everting the eyelids, using slit lamp if possible. See Eye examination
- Stain with fluorescein to assess for corneal abrasion. Apply 1 drop to each eye, or for strips; wet strip with 0.9% sodium chloride and touch to lower lid only
- Remove small foreign body with moistened cotton bud. A 25 gauge needle with bevel up may be used in older, cooperative children, using slit lamp while approaching the child from the temporal aspect of the eye
- For larger defects (>2 mm) apply chloramphenicol 1% ointment and double eye-pad overnight. For smaller defects (
<2 mm) apply chloramphenicol 0.5% drops four times per day for 5 to 7 days
- Need daily review (visual acuity and slit lamp examination) until epithelium healed
- For persistent pain (>48 hours) or no improvement, seek ophthalmology advice
 |
 |
Corneal abrasion in child’s right eye from finger nails

|
|
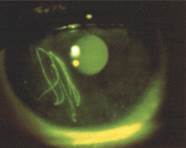
Corneal metal foreign
body with rust ring |
Linear corneal abrasions
suggestive of a subtarsal foreign body |
Chemical (strong acid/ alkali) burns
- Urgent, copious irrigation, after local topical anaesthetic, including under top lid. Sedation or urgent GA may be required
- Particulate alkaline matter needs urgent, total removal with a cotton bud
- Use 3 litres of 0.9% sodium chloride through an open giving set over about 15 minutes
- Irrigate from 3-5 cm above the ocular surface. Ask the child to look left, right, up and down whilst irrigating
- Continue irrigation until pH normal (6-8). Measure pH using universal indicator paper in the conjunctival fornix
- Discuss all burns with the ophthalmologist
 |
|
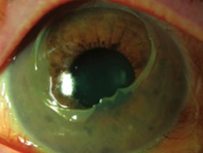
Acute alkali chemical injury
(mild/moderate) |
Chemical/thermal injury (severe with
corneal epithelial defect and opacity) |
Reproduced with permission from The Royal Australian College of General Practitioners from: Lu SJ, Lee GA, Gole GA. Acute red eye in children: A practical approach. Aust J Gen Pract 2020;49(12):815–22 doi: 10.31128/AJGP-02-20-5240.
Thermal burns
- First aid takes precedence over a complete examination
- Local anaesthetic and copious irrigation. See
chemical burns above
- Discuss all eye burns with the ophthalmologist
Lid laceration
- Treat as a potential penetrating injury until proven otherwise, see
Penetrating eye injury
- Superficial laceration away from the lid margin, may be safely closed by standard suture techniques
- Any laceration that involves the eye lid margin should be repaired by an ophthalmologist
Contact lens associated red eye
- Anaesthetise eye and remove contact lenses if possible
- Stain eye and check for corneal abrasions or foreign body
- Swab if discharge present, Gram-negatives including P. aeruginosa are frequently the cause, thus requiring broader-spectrum antibiotics
- If ulcer identified refer urgently to ophthalmology
- Start topical chloramphenicol (1% ointment or 0.5% drops) and arrange for follow-up
Subconjunctival haemorrhage
- If localised, may suggest penetrating injury (but can be due to Valsalva manoeuvre)
- If the posterior extent of the haemorrhage cannot be visualised, an orbital or base of skull fracture is possible
- In infants, subconjunctival haemorrhage may be a sign of non-accidental injury, see
Child abuse
Acute eye injury

Consider consultation with local paediatric team when
A child with suspected child abuse or neglect, significant associated trauma, or medical instability
Consider consultation with ophthalmology:
- A child with:
- A sight threatening condition
- A large corneal foreign body, or one that is difficult to remove
- If required to facilitate a complete examination particularly in distressed child
- If retinal assessment and photography is required for suspected child abuse
Consider transfer when
- A child with a sight threatening condition and/or management is beyond the capacity of the local team
- A child with significant other major injuries that require tertiary or specialist care
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
- Normal eye examination and nil other symptoms
or
- Sight threatening conditions are excluded AND
- Appropriate treatment instituted for minor injuries AND
- Follow up, or early review criteria provided to child and family
Additional notes
The
Eye Emergency Manual App provides clinical guidelines for the management of eye emergencies and provides a ‘paediatric filter’
Last updated October 2022