See also
Burns - Post Acute Care and Dressings
Key points
- Burn injuries should be managed as a Trauma case requiring primary and secondary survey
- Accurate Total Body Surface Area (TBSA) estimation is essential for fluid resuscitation decision making. TBSA does not include epidermal burns
- Ensure adequate analgesia to facilitate assessment and patient comfort
- Appropriately consented photographs of the burn are very helpful for assessment and monitoring
Background
Specific features in children with burns
- Children have thinner skin than adults, predisposing them to a deeper burn for any given temperature
- Assessment of burn depth is difficult, especially early post injury
- Young children are at risk of hypothermia, especially during initial cooling of the burn
Burns are described as epidermal, dermal (superficial/mid/deep) and full thickness
Assessment
History of burn
- Time of injury
- Mechanism of injury, including circumstance for specific pattern of burn
- Scald: estimated temperature and nature of the liquid
- Contact: estimated temperature and nature of the surface
- Friction
- Flame / explosion: product that burned/exploded, location (enclosed vs. open space); duration of exposure, inhalation injury
- Electrical: voltage, type of current (AC or DC), duration of contact
- Chemical: type of product
- Cold: direct contact with cold surface or exposure (frostbite)
- Radiant: sunburn
- First aid
- Time started (was it within 3 hours and maintained)
- Agents used
- If clothes and jewellery were removed
- Decontamination method (for chemical exposure)
- Consider co-existing non-burn injuries
- Consider
non-accidental injury or vulnerable child
- Tetanus status
Examination and initial management
Like all traumas paediatric burn assessments require a primary and secondary survey with the initial aim of identifying and managing immediate life threats: do not get distracted by the burn injury.
Airway
- Signs of airway burn/inhalation injury: stridor, hoarseness, black sputum, respiratory distress, singed nasal hairs or facial swelling
- Sign of oropharyngeal burn: soot in mouth, intraoral oedema and erythema
- Significant neck burn
- If above present, consider early intubation
- If suspicion of airway burns or carbon monoxide intoxication apply high flow oxygen
- Protect the cervical spine with immobilisation if there is associated trauma
Breathing
- Full thickness and/or circumferential chest burns may require escharotomy to permit chest expansion
Circulation
- If early shock is present, consider causes other than the burn
- IV fluid resuscitation as required
- IV or IO access (preferably 2 points of access)
- For circumferential burns check peripheral perfusion and need for escharotomy
Disability
- If altered conscious state, consider airway support
- Assess neurovascular status if limb involved
Exposure - burn assessment and initial management
- Assessment of burn depth
- Burns are dynamic wounds, it is difficult to accurately estimate the true depth and extent of the wound in the first 48-72 hours
- Do NOT include area with epidermal burn (erythema only)
|
Classification
|
Depth
|
Colour
|
Blisters
|
Capillary Refill
|
Sensation
|
|
SUPERFICIAL
|
Epidermal
|
Red
|
No
|
Brisk
|
Present
|
|
Superficial Dermal
|
Pale Pink
|
Present
|
Brisk
|
Painful
|
|
Mid Dermal
|
Dark Pink
|
Present
|
Sluggish
|
+/-
|
|
DEEP
|
Deep Dermal
|
Blotchy Red
|
+/-
|
Absent
|
Absent
|
|
Full Thickness
|
White
|
No
|
Absent
|
Absent
|
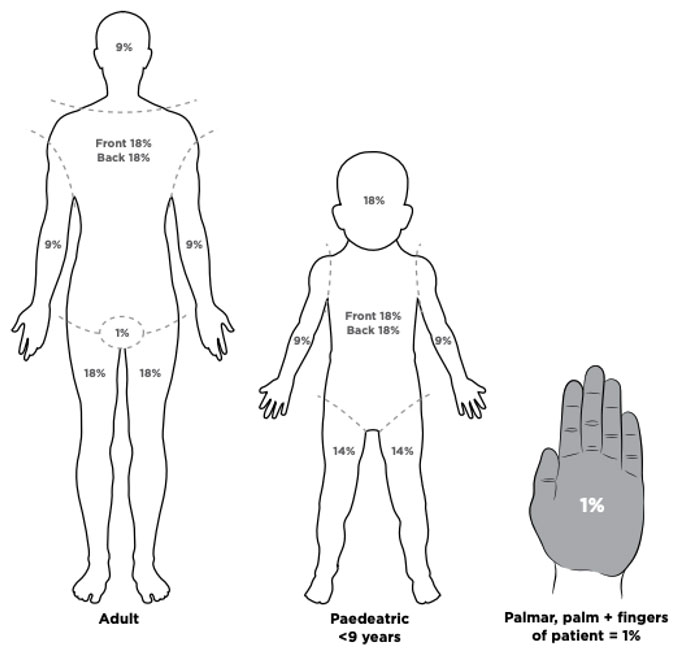
- Assessment of TBSA
- Expose whole body - remove clothing and log roll to visualise posterior surfaces
- Use Lund & Browder Chart
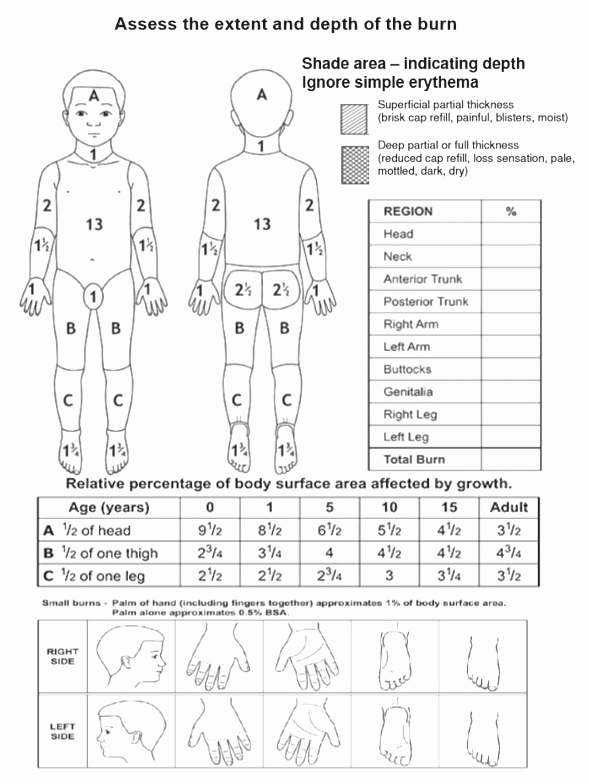
- The palmar surface of the child’s hand (including fingers) represents approximately 1% TBSA and can be used to approximate TBSA
- First aid
- Remove jewellery and clothing in contact with burn source
- Cool affected area as soon as possible (within 3 hours from time of burn) for 20 minutes with cool running water
- If unavailable, other options include: frequently changed cold water compresses, immersion in a basin, irrigation via an open giving set
- Never apply ice and avoid use of hydrogel burn products
- Cover burn with plastic cling film lengthways along the burn (do not wrap circumferentially)
- Do not apply plastic cling film to face (use paraffin ointment)
- Do not apply plastic cling film to a chemical burn
- Discuss chemical burn decontamination with Poisons Information (Tel: 131126)
- Appropriately consented photos of burns prior to dressings are useful for ongoing management
- Prevent hypothermia
- Remove wet clothes/dressings after initial cooling
- Try to keep child otherwise warm
- Cover the wound and the child after assessment
- When possible, warm intravenous fluids and the room
Fluid management in burns ≥10% TBSA
The goal is management of burns shock, through optimal replacement of fluid losses to maximise wound and body perfusion, and minimise wound and body oedema and associated adverse effects
- Calculate requirements from time of the burn, not time of presentation
- Calculate fluid volume using Modified Parkland Formula (see below)
- Hartmann’s Solution is the fluid of choice - if unavailable, use 0.9% sodium chloride
- Insert urinary catheter for strict fluid balance
- Keep nil by mouth and consider nasogastric tube - gastric ileus is a potential complication
Modified Parkland Formula
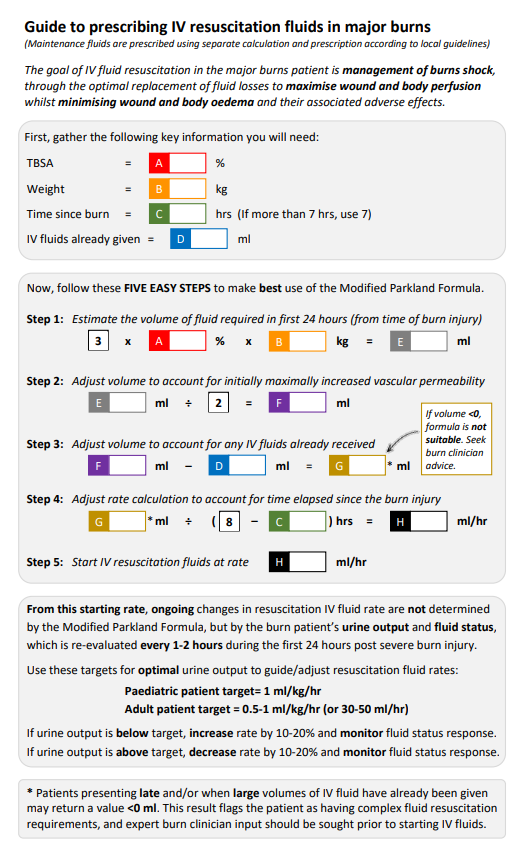
Patients with delayed fluid resuscitation, electrical conduction injury and inhalation injury have higher fluid requirements. Discuss with specialist team
Analgesia
- Especially during cooling, dressing and mobilisation. See
Acute Pain Management
- Appropriate initial choices include intranasal fentanyl or IV morphine
Initial investigations
|
Major burn (≥10% TBSA)
|
Haemoglobin, electrolytes, BGL, group and hold, VBG
|
|
Multi trauma
|
See
Primary and Secondary survey
|
|
Suspected inhalation injury
|
ABG for carbon monoxide
|
|
Electrical burn
|
ECG
|
Burn wound management
FACADE = First aid, Analgesia, Clean, Assess, Dress, Elevate
General burn management
- Limit debridement to wiping away clearly loose/blistered skin
- De-roof blisters with moist gauze or forceps and scissors if >5mm or crossing joints. See
blister management
- Clean burn wound and surrounding surface with saline or water
- Reassess burn, take photos with appropriate consent
- Apply appropriate occlusive non-adherent
dressing. If these products are not available, refer to local Burns service for alternative options
- If there is anticipated delay or time until definitive care, consider use of multiple layer BactigrasTM
|
Location
|
Depth
|
Dressing
|
|
Facial and perineal burns
|
Epidermal or superficial dermal
|
Apply white soft paraffin twice daily after cleaning face
Chloramphenicol ointment to eye and ear burns
Perineal burns are at risk of contamination – after bowel action, area should be cleaned with soapy solution; consider catheterisation
|
|
Mid or deep dermal
|
Consider silver-impregnated dressing (discuss with Burns service)
|
|
Other body regions
|
Epidermal
|
May not require dressing
Consider covering with protective, low-adherent dressing (eg MepitelTM, MelolinTM, BactrigrasTM) for comfort
|
|
Mid or deep dermal
|
Dressing product used depends on the expected duration required before removal or wound review
|
Consider consultation with local paediatric team when
- Suspected non-accidental injury, self-inflicted burns or assault
- Multiple co-morbidities
- Concern regarding ability to care for burns at home
Consider transfer when
Child requiring care beyond the comfort level of the hospital
Following burns:
- >10% TBSA
- All full thickness
- Special areas: face, ears, eyes, neck, hands, feet, genitalia, perineum or a major joint, even if
<10%
- Circumferential
- Chemical
- Electrical
- Associated with trauma and/or spinal cord injury
- All inhalation/airway
- Children
<12 months
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Special considerations
|
Type of burn
|
Consideration
|
|
Circumferential deep burn (deep dermal or full thickness)
|
Neurovascular compromise
Elevate part of limb distal to burn
Monitor colour, capillary refill time, temperature
Escharotomy may be required
|
|
Head and neck burns
|
Nurse head up to reduce swelling and oedema
|
|
Ocular burns (See
Acute eye injuries in children)
|
Signs include blepharospasm, tearing, conjunctivitis
All facial burns should have assessment with fluorescein 2% eye drops to assess for corneal damage
Treat with copious irrigation using 0.9% sodium chloride with topical anaesthetic in eye (unaffected eye upwards)
- Up to 1 hour with acidic contamination or until pain stops
- Up to 2 hours with alkaline contamination or until pain stops
Topical chloramphenicol to prevent secondary infection
Urgent paediatric ophthalmology review
|
|
Limb burns
|
Elevate the limb
Monitor perfusion distal to burn
|
|
Suspicion of associated Carbon monoxide (CO) poisoning, Cyanide poisoning
|
Liaise early with Paediatric Burn Unit, Intensive Care and Poisons Information (Tel: 131126)
|
|
Electrical injuries
|
Liaise early with Paediatric Burn Service and Intensive Care
Inspect for entrance/exit wounds
Consider spinal precautions
Risk of dysrhythmias - consider 24 hours ECG monitoring
Monitor for elevated CK, urine haemoglobin and haemochromogen
|
Chemical burns
- Personal protective equipment for first aid givers should be worn (gloves, mask, gown, eye protection)
- Remove contaminated clothing
- Brush powdered agent off skin
- Areas in contact with chemical should be irrigated with cool water
- Irrigate to floor with appropriate drainage so contaminated water does not cause further injury
Tetanus prone wounds
Parent information
Burns – medical treatment
Burns – prevention and first aid
Burns – rehabilitation
Additional notes
See individual State Burns and Trauma clinical information and mobile phone applications
Last updated June 2020