See also
Acute behavioural disturbance: Acute management
Engaging with and assessing the adolescent patient
HEEADSSS interview
Mental state examination
Substance use (abuse)
Key points
- Most young people do not require medication on cessation of cannabis, rather coping strategies, information and reassurance
- Nicotine co-dependence is common amongst cannabis users, so nicotine withdrawal should be concurrently treated
- Withdrawal may be more severe in those with psychiatric co-morbidities and psychosocial vulnerabilities
- Cannabis withdrawal may not be the presenting complaint and can occur in the context of any young person's admission
- Plan ongoing care by linking with post-withdrawal services
Background
- Cannabis use is common in young people
- Cannabis withdrawal syndrome (CWS) is a well-characterised phenomenon which occurs in heavy cannabis-users (daily or almost daily use over months) after abrupt cessation or significant reductions in cannabis use
- Around one in six young people who ever use cannabis may develop symptoms of dependence, such as increased tolerance, difficulty cutting down or experiencing withdrawal symptoms when decreasing or stopping use
- CWS typically occurs 1-2 days after last use. The acute phase symptoms peak at day 2-6. Symptoms usually subside after 2-3 weeks but some symptoms eg sleep disturbance may persist for months
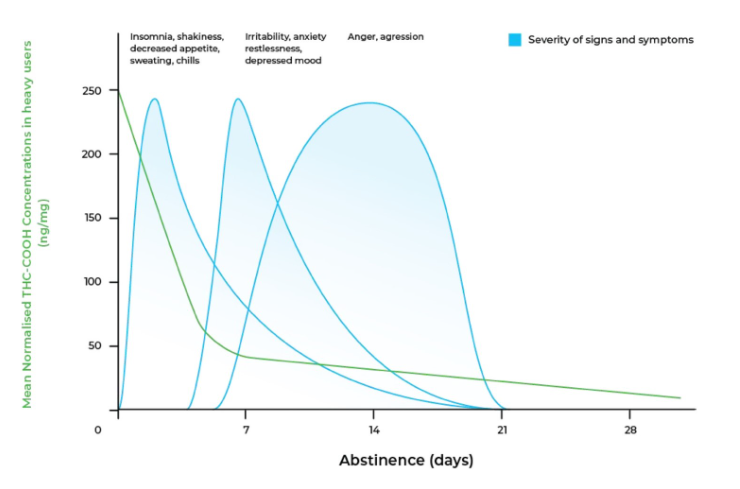
Figure 1. Typical course of cannabis withdrawal. Adapted from Goodwin et al. and Queensland Health (2012)
- A young person’s presentation may be planned (elective withdrawal) or unplanned, eg being hospitalised for treatment not related to cannabis use
- Most dependent cannabis users have concurrent dependence to nicotine due to the common practice of mixing cannabis with tobacco. Withdrawal from both nicotine and cannabis can lead to more severe withdrawal symptoms
- Cannabis hyperemesis syndrome is a condition characterised by recurrent, severe nausea. It is associated with regular cannabinoid use rather than being a withdrawal syndrome. It should be differentiated from CWS and managed with IV fluid hydration, antiemetics, dopamine antagonists and topical capsaicin cream
Assessment
History
- Common features of cannabis withdrawal
- Irritability
- Insomnia
- Anxiety
- Low mood
- Aggression
- Decreased appetite
- Nausea
- Headache
- Less common features: chills, sweating, tremor, abdominal pain
- Pattern of use: Frequency, quantity, method of consumption (joint/bong/e-cigarette/cookies/gummies), timing of last use
- High risk of withdrawal if daily or almost daily use over several months
- Polysubstance use, including tobacco (nicotine), alcohol, stimulants (ice, cocaine, MDMA), benzodiazepines, opioids (heroin, prescription opioids), inhalants (nitrous oxide/‘nangs’, chroming), hallucinogens (LSD)
- Characteristics of any previously experienced withdrawal symptoms and their severity
- Physical health issues
- Mental health issues, including symptoms of psychosis
- Pregnancy
- Young person's psychosocial screen (HEEADSSS interview)
Factors associated with severe withdrawal
- Previous complex withdrawal eg aggression, suicidal ideation or attempt, or psychosis
- Polysubstance dependence
- Co-occurring mental health disorders or medical conditions (eg T1DM, IBD)
Examination
- Vital signs
- Physical exam to identify signs of intoxication/withdrawal
- Mental state examination
- The Cannabis Withdrawal Assessment Scale can assist with assessment of the nature and severity of cannabis withdrawal. However, it is not validated for the use of medications in response to symptoms (see Additional notes)
Management
A collaborative approach with the young person, which empowers them with information and self-efficacy, is key to developing a successful management plan
Opportunistic vaccinations should be offered if not up to date, including Hepatitis B and HPV (consider hepatitis A)
Investigations
- Opportunistic sexual health, pregnancy and blood-borne viruses screen
- Urine drug screens should not be routinely performed
- Note: cannabinoids can persist in the urine for several weeks after cessation of use
Treatment
Management is supportive and non-pharmacological for the vast majority. There is no standard medication regimen for cannabis withdrawal. Rather, short-term PRN medications are prescribed for symptom management
1st line non-pharmacological
|
Strategy
|
Notes
|
Resources
|
|
Psychoeducation
|
Most young people do not require medication on cessation of cannabis, rather coping strategies, information and reassurance
Educate young person and their carers regarding common withdrawal symptoms, their likely onset, duration and coping strategies
|
For young person:
What is cannabis - Headspace
For families/carers:
Cannabis use and young people - Alcohol and Drug Foundation
|
|
Coping with cravings
|
A craving is a strong desire to use a substance. Cravings are normal and they will pass
Cravings can be described to the young person like an ocean wave - "it starts off small, gathers momentum, peaks, and then breaks. Cravings are time limited. The trick is to ride out the peak until it passes" (urge surfing)
|
Turning point: understanding and managing cravings
Understanding cravings
Coping with cravings
Nicotine cravings - what to do when craving a vape or cigarette
Strategies
- The 3 D’s (delay, distract, deep breathing)
- Urge surfing
- Mindfulness strategies
- Consider other common causes of cravings (HALTs: Hunger, Anger, Loneliness, Tiredness)
|
|
Coping with irritability, anger, agitation, restlessness
|
Environmental stressors can have a significant effect on the severity of withdrawal. Minimise stress by ensuring that the environment is quiet, calm, safe and private
Help the young person identify potential triggers, as well as strategies that soothe
|
Youth Recovery Toolkit, Substance & Alcohol Abuse Help for Youth
SMART Tool Enjoyable Activities Checklist
|
|
Coping with reduced appetite
|
Many young people have reduced appetite during cannabis withdrawal, which together with nausea and poor hydration can result in dehydration.
Recommend the young person try to maintain small regular light meals over the course of the withdrawal episode, and to maintain hydration
|
|
|
Coping with insomnia
|
Sleep issues are a common struggle in recovery from substance dependence and can be five times higher in early recovery than in the general population. It is important to recognise this as a common cause for relapse and discuss strategies
with the young person
|
How to improve your sleep while in addiction recovery
Tips to help young people sleep better
Tips for Supporting Better Sleep by Black Dog Institute
|
2nd line pharmacological (short-term)
|
Symptoms
|
Medication
|
Notes
|
|
Pain/headaches
|
Paracetamol 15 mg/kg (max 1 g) qid prn
Ibuprofen 10 mg/kg (max 400 mg) tds prn
Hyoscine butylbromide for abdominal cramps
|
|
|
Nausea and vomiting
|
Ondansetron 0.15 mg/kg (max 8 mg) orally tds prn
Cyclizine 1 mg/kg (max 50 mg) 8 hourly orally/IV/IM
Metoclopramide 10 mg tds prn
|
Caution: risk of EPSE with metoclopramide use
|
|
Severe withdrawal/agitation
|
Diazepam 5 mg orally qid prn (max 20 mg in 24 hours)
Higher doses of diazepam may be required for some young people, use with appropriate clinical supervision
|
Senior clinician review
Wean over 5-7 days
There are risks involved in introducing young people to benzodiazepines, hence caution must be used in prescribing them. They should not be prescribed in the outpatient setting without specialist consultation
|
|
Severe withdrawal not responding to diazepam
|
Olanzapine 2.5-5 mg orally bd prn
|
Use diazepam before using olanzapine
Seek specialist advice
|
|
Insomnia
|
Melatonin 2-5 mg oral nocte
|
|
|
Nicotine withdrawal
(if concurrent nicotine dependence)
|
Nicotine replacement therapy
Combination of long-acting (patch) + short-acting (lozenge, inhaler, gum, spray) is most effective
|
Refer to AMH Children’s Dosing on nicotine replacement therapy
Tools for health professionals on Tobacco and smoking
Nicotine Replacement Therapy and Adolescent Patients
|
Ongoing care
Linking the young person with relevant voluntary services post-withdrawal is associated with improved outcomes. Increasing awareness of available support services is an important element of providing
care
Post-withdrawal services include:
- Drug and alcohol services for youth
- Family drug support services
- Peer-support groups (SMART Recovery)
- Mental health services
- General practitioners
- Accommodation services
- Child protection agencies
- Legal services
Consider consultation with local paediatric team when
- Withdrawal is more severe or complex due to polysubstance use, concurrence of mental ill-health, physical, neurodevelopmental and/or psychosocial co-morbidities
- Needing assistance in determining appropriate treatment context for young person (outpatient, inpatient, drug and alcohol unit, mental health unit)
- Needing assistance in titrating sedating medications
- Concerns about young person’s safety due to drug and alcohol use
Consider transfer when
- Young person requires tertiary-level mental health care
- Care above the comfort of the local health service
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
Clear plan for follow-up is in place which address drug and alcohol as well as psychosocial concerns
Patient information
Cannabis information and support
Additional resources
Phone service for health professionals seeking advice from addiction medicine specialists:
Additional resources for health professionals
Insight - Toolkits - Withdrawal Management
Headspace clinical toolkit
Additional notes
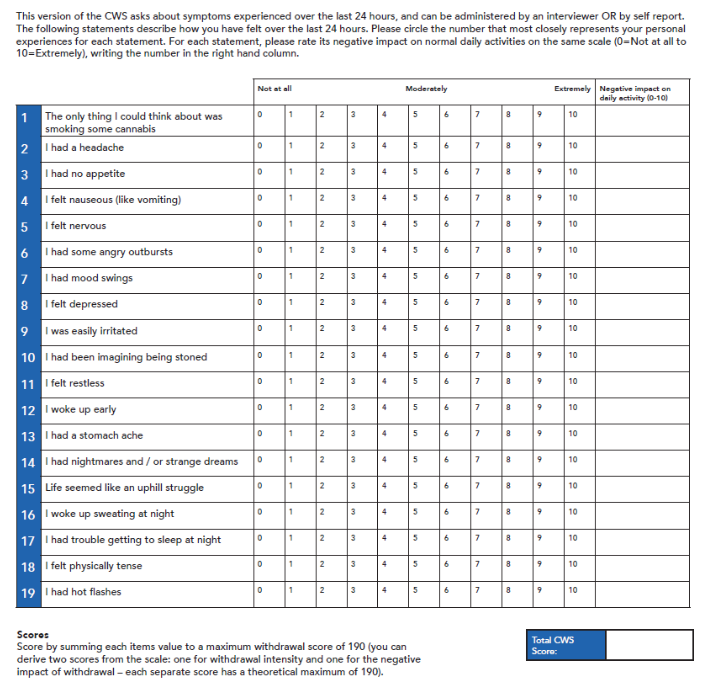
Figure 2. Cannabis withdrawal scale by Allsop et al
Last updated December 2024