See also
Dental conditions - non traumatic
Trauma - primary survey
Lacerations
Key Points
- Management of dental trauma depends on whether primary or permanent teeth are involved
- Injuries to primary teeth are generally managed by observation or extraction
- Successful replantation of permanent teeth or teeth fragments requires urgent management to improve long term tooth viability
Background
- Dental trauma is very common, and often occurs alongside other injuries, especially facial and head injuries. Where required, perform a primary and secondary survey prior to instituting dental management
- Management of dental trauma is different for primary (baby) teeth compared to permanent teeth, as primary teeth are never repositioned, splinted or replanted
- Severe injuries to primary teeth can cause later problems in the formation and eruption of permanent teeth. Treatment of injuries to primary teeth is aimed at minimising additional risks to the developing permanent teeth and preventing complications
such as aspiration of tooth fragments
- Crown discolouration is a common complication after dental injury. This may resolve with time. Extraction is only required where there is associated infection of the dental pulp or abscess formation
- Appropriate use of a mouthguard during sports can minimise dental trauma
- In young children and infants with oral trauma, consider child abuse
Assessment
Reviewing tooth anatomy, tooth numbering and
eruption dates will assist when referring to dentist
History
- Mechanism of injury and associated injuries
- Time since injury - avulsion of a permanent tooth is a dental emergency
- First aid rendered - tooth rinsing, wet or dry storage
- Sensitivity to hot and/or cold
- Previous dental history including injuries, crowns or prostheses
- Tetanus immunisation status
Examination

- Use the "lap-to-lap" position for toddlers
- Check symmetry in the mouth and alignment of teeth
- Lift the lips to look for gingival or oral mucosal injury
- Type of tooth and whether permanent or primary
- Type of dental injury: loose or displaced tooth, fractured tooth, injury to supporting bone, injury to oral mucosa or gingivae
- Bite for even occlusion, subjective or objective; steps in bite or bone border
- Temporomandibular joint movement and tenderness
- Numbness, intra or extraoral bruising
- Account for all lost teeth and fragments, examine chest and soft tissues of the mouth if any missing as they may have been aspirated or embedded
Management
Investigations
- Orthopantogram (OPG) for children >3 years who can cooperate if considering fractured mandible, temporomandibular joint (TMJ) injury or concern for fully intruded tooth
- Chest x-ray if suspicion of aspiration of missing tooth or fragments
- Occlusal (bite-down) views can only be done by dental service
Treatment
- Discuss with emergency dental service and provide an intraoral photograph of the injury, where possible. They will assess the injury and determine whether emergency specialist management or referral to a community dental clinic for non-urgent assessment
is required
- Prophylactic antibiotics recommended after replantation of avulsed tooth, soft tissue injuries with debris or operative management required. Provide tetanus booster if
required
- Healing after a dental injury requires good oral hygiene. Swabbing the area with 0.12% chlorhexidine mouth wash twice a day for 10-14 days reduces the infection risk. A soft diet will also allow loose teeth to become firmer
Loose or displaced teeth
| Injury |
Examination findings
|
Management
|
|
Concussion
|
Tender but firm
|
Review by community dentist
Usually heal without intervention
|
|
Subluxation
|
Tender loose tooth, blood around gum
|
Refer to emergency dental service if very loose
|
|
Lateral luxation
Extrusion
Intrusion
|
Anteriorly or posteriorly displaced
Partially out of socket
Pushed into socket
|
Refer to emergency dental service
Primary: monitored or extracted
Permanent: usually repositioned or splinted under local or general anaesthetic
|
|
Avulsion
|
Complete displacement from socket
Note: need to differentiate avulsion from fully intruded tooth (may need x-ray)
|
Refer to emergency dental service
Primary: not reinserted
Permanent: place in milk (1st choice) or saline while awaiting assessment
Do not store tooth in water or scrub tooth
Handle the crown (white) only, do not handle tooth root (yellow)
If possible, return to socket and bite down with gauze to hold tooth in position. Support tooth with alfoil wrap
Best prognosis if "dry-time"
less than 20 minutes
Prophylactic antibiotics indicated after replantation
|

Fractured teeth
Enamel is white, dentine is yellow, pulp is pink
|
Injury
|
Examination findings
|
Management
|
|
Enamel fracture,
Enamel-dentine fracture
|
Fracture confined to enamel +/- dentine
|
Review by community dentist
|
|
Enamel-dentine-pulp fracture
|
Fracture with exposure of pulp (pink and painful)
|
Refer to emergency dental service
Primary: for likely extraction
Permanent: keep tooth fragments in milk for possible rebonding
|
|
Crown-root fracture
|
Fracture in crown extending below gums. May be aspiration risk
|
Refer to emergency dental service
|
|
Root fracture
|
Displacement or mobility of tooth
|
Refer to emergency dental service
|

Injuries to the supporting bone
- Check that the child's bite is normal
- Get an OPG and other views as required
- Refer to both dental and maxillofacial (obvious jaw fractures)
- Dental and maxillofacial follow-up is recommended for all patients with mandibular or maxillary fractures, even when undisplaced
Injuries to the gingivae or oral mucosa
- Oral mucosa degloving injuries (gingivae stripped from underlying bone) can be missed if the lips are not firmly lifted away from the gum as part of the examination
- The chin is often swollen and tender in mandibular degloving injuries
- Degloving injuries and deep lacerations or tears require operative cleaning, debridement and suturing to reduce the risk of osteomyelitis
- Refer to emergency dental service
- Manage intra and extraoral lacerations as required
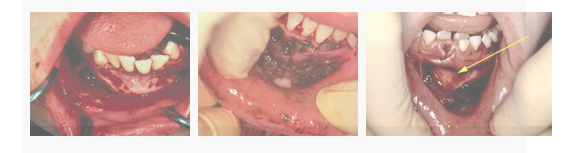
Oral mucosal degloving injuries
Consider consultation with local paediatric dental team when
Dental trauma requiring surgical input and assessment
Consider transfer when
Specialist dental or maxillofacial assessment and management is required and is not locally available
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
Intervention is complete and follow up plans are in place
Parent information
Broken or dislodged tooth
Dental care
Additional notes
International Association of Dental Traumatology Dental Trauma Guide
Access to dental services
Each state has eligibility criteria for access to public dental services
Some children will also be eligible for the Child Dental Benefits Schedule which subsidises dental treatment through public or private dental services
Last updated July 2024