See also
Acute otitis media
Meningitis and encephalitis
Head injury
Key points
- Children presenting with headache require careful assessment for red flag features, in order to detect serious underlying secondary causes
- Most children presenting with headache do not require investigations
- Supportive therapy with simple analgesia is the mainstay of treatment for most cases of primary headache; opioids are not recommended
Background
- Headaches can be classified as primary (intrinsic to the nervous system) or secondary (due to another underlying condition)
- The most common primary headaches in children are migraine and tension-type headache
- Viral illnesses are the most common cause of secondary headaches in children, while less common but serious causes include CNS infection (meningitis, encephalitis), raised intracranial pressure and haemorrhage
- Headache may also be a manifestation of underlying psychosocial issues
Assessment
History
Consider red flags:
- Age
< 4 years
- Headache features (any)
- Early morning
- Wakes the child from sleep
- Triggered or aggravated by coughing, sneezing or positional changes (eg bending forwards)
- Sudden onset and severe
- Occipital region
- Associated vomiting without another clear cause
- Significant change in an established headache pattern or progressive worsening
- Focal neurological symptoms
- New onset
seizures
- Developmental regression
- Features of
meningitis or encephalitis
- Recent history of significant
head injury
- Known systemic disorder: haematological condition (bleeding tendency, prothrombotic state), malignancy, rheumatological disorder, immunosuppression, hypertension
- Medications: anticoagulants, antiplatelet agents
- Presence of ventriculoperitoneal (VP) shunt
Other features
Headache patterns
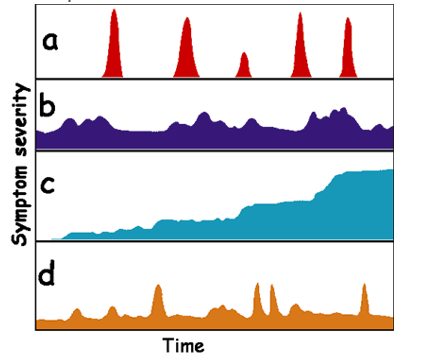
- Acute recurrent
- Chronic non-progressive
- Tension-type headache
- Anxiety, depression
- Somatisation
- Chronic progressive
- Tumour
- Benign intracranial hypertension
- Brain abscess
- Hydrocephalus
- Acute on chronic non-progressive
- Tension headache with co-existent migraine
Common migraine triggers include:
- Illness
- Poor sleep
- Exercise
- Menstruation
- Stress
- Heat
- Sun glare
- Foods: citrus, MSG, artificial sweeteners, nuts, onions, salty foods, caffeine, chocolate
- Skipped meals
- Missed medications or medication overuse
Examination
Observations including BP and conscious state
Neurological examination – cranial nerve and peripheral nerve examination, gait, fundoscopy
Stigmata of neurocutaneous syndromes (eg neurofibromatosis, tuberous sclerosis)
Red flag findings include:
- Altered conscious state/confusion
- Increasing head circumference centiles
- Abnormal head position
- New focal neurological abnormalities
- Signs of raised ICP (papilloedema, ataxia, bradycardia with hypertension)
- Signs of meningism (photophobia, neck stiffness)
Primary Headache
| Headache feature |
Tension-type headache |
Migraine with or without aura |
Cluster headache |
|
Age |
All ages |
All ages |
Typically ≥12 years of age |
|
Pain location |
Bilateral |
Unilateral or bilateral |
Unilateral, often around the eye |
|
Pain quality |
Pressing/tightening (non-pulsatile) |
Pulsatile |
Variable (sharp, burning, throbbing or tightening) |
|
Pain intensity |
Mild to moderate |
Moderate to severe |
Severe to very severe |
|
Headache pattern |
Chronic non-progressive |
Acute recurrent |
Acute recurrent |
|
Effect on activities |
Not exacerbated by activity |
Aggravated by normal activities |
Can cause restlessness and agitation |
|
Associated symptoms |
None
May be precipitated by significant stress ie emotional distress, poor sleep, missed meals |
Nausea and vomiting, photophobia, phonophobia
With aura: presence of focal neurological symptoms, usually visual, sensory or speech changes before onset of headache (aura lasts less than one hour) |
Autonomic symptoms ie ipsilateral conjunctival injection, tearing, rhinorrhoea, eyelid swelling, facial sweating, meiosis or ptosis |
|
Duration |
Hours to days |
May only last 30 minutes in young children, up to 72 hours in adolescents |
Minutes to a few hours |
Secondary Headache
| Causes |
Specific conditions to consider |
|
Infectious |
Viral illness
Sinusitis
Pharyngitis
Acute otitis media
Meningitis
Encephalitis
Intracranial abscess
Dental caries |
|
Headache associated with trauma |
Head injury |
|
Raised intracranial pressure (ICP) |
Idiopathic intracranial hypertension
Hydrocephalus
Intracranial neoplasm
Other intracranial malformations |
|
Vascular |
Stroke
Intracranial haemorrhage |
|
Drug related |
Substance use/withdrawal
Medication overuse |
|
Psychiatric disorder |
Anxiety
Depression
Somatisation disorders
Increased psychosocial stressors
See
Mental state examination |
Management
Investigations
Investigations are not routinely indicated in children with headache presenting without red flag features on history or examination
If red flags present, discuss with a senior clinician and consider intracranial imaging
Treatment of primary headaches
General advice
- Ensure adequate hydration
- Encourage good sleep hygiene and a healthy exercise pattern
- To prevent medication overuse headache, limit use of simple analgesics to less than 15 days per month, and triptans to less than 10 days per month
- Avoid triggers
- Address emotional stressors which may be precipitating the headache
- A
headache diary or App can be used to monitor response to lifestyle modifications and treatment
Tension-type headache
- Provide simple
analgesia
- Paracetamol 15mg/kg (max 1g)
- Ibuprofen 10mg/kg (max 400mg)
- Manage triggers
- Opioids should not be offered for the acute treatment of tension-type headache
Migraine headache
Soon after onset of migraine (usually at home)
- Paracetamol 15mg/kg (max 1g)
- Ibuprofen 10 mg/kg (max 400 mg)
- Keep hydrated and rest/sleep in quiet, dark room
- Rizatriptan (wafer or disintegrating tablet) may be used if oral analgesics ineffective (sumatriptan nasal spray is no longer available)
- >6 yo and <40 kg: 5 mg orally
- >40 kg: 10mg orally
- can be repeated once after 2 hours if headache recurs (max 2 doses in 24 hours)
- Propranolol increases the plasma concentration of rizatriptan - avoid or use lower doses of rizatriptan (seek specialist advice)
- Avoid opioids in the treatment of migraine
On presentation to ED consider
- Paracetamol and ibuprofen, if not already given
- Ondansetron 0.15 mg/kg (max 8 mg) oral/IV if vomiting
- If ≥8 yo:
- IV Chlorpromazine (Largactil) 0.25 mg/kg (max 12.5 mg) in 10–20 mL/kg sodium chloride 0.9% (max 1 L) administered over 30-60minutes
OR
IV Prochlorperazine (Stemetil) 0.15 mg/kg (max 10mg) in 10-20 mL/kg sodium chloride 0.9% (max 1L) administered over 30-60 minutes - both agents may cause hypotension and require BP monitoring and administration with IV fluid (as above) +/- additional IV fluids
- Rest/sleep in a dark, quiet cubicle
- Therapeutic nerve blocks may be offered by experienced ED clinicians, or by anaesthetic/pain specialists
Cluster headache
- Simple analgesia has not been shown to be effective
- Administer 100% oxygen with a flow rate of at least 12 L per minute via a non-rebreathing mask with a reservoir bag
- Rizatriptan (wafer or disintegrating tablet)
- >6 yo and <40 kg: 5 mg orally
- >40 kg: 10mg orally
- can be repeated once after at least 2 hours if headache recurs (max 2 doses in 24 hours)
- May have a secondary cause, suggest a low threshold for neuroimaging
Consider consultation with local paediatric team when
A child presents with headache and a red flag symptom/sign
Consider transfer when
Neurosurgical intervention required or child requiring escalation in care beyond the comfort of the local healthcare facility
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
- Child is clinically stable and no red flag features
- Appropriate follow-up has been arranged
Migraine discharge planning and follow up
- It is unlikely that a migraine headache will fully resolve in the emergency department
- On discharge home, encourage the child to continue resting in a quiet, dark environment to enable recovery
- GP follow up or referral to a paediatrician may be appropriate for ongoing management of headaches including consideration of preventative treatments
Parent information
Headache
Migraine
Head injury
Last updated December 2022