See also
Diabetic ketoacidosis
Diabetes mellitus
Diabetes mellitus and surgery
Key points
- Hyperosmolar hyperglycaemic state (HHS) is a medical emergency of serum hyperosmolality, hyperglycaemia and dehydration without ketoacidosis
- All children with HHS require urgent consultation with a senior clinician, ICU or relevant retrieval team
- The management of HHS differs to that of diabetic ketoacidosis (DKA). HHS also carries a higher morbidity and mortality than DKA
- The first step in management is aggressive fluid resuscitation followed by replacement and monitoring of electrolytes. Only administer insulin following fluid resuscitation; a rapid fall in serum glucose causes critical fluid shift and electrolyte
derangement
Background
- HHS is a complication of diabetes and results from a relative lack of insulin resulting in a triad of severe hyperglycaemia, high serum osmolality and severe dehydration, without marked ketoacidosis
- This results in a fluid shift from the intracellular to extracellular space, electrolyte derangement and severe hypertonic dehydration
- Unlike DKA, relatively sufficient insulin prevents significant lipolysis, and so ketoacidosis is not a feature (although occasionally hypoperfusion
secondary to severe dehydration results in mild non-ketotic acidosis)
- In comparison to DKA, dehydration and electrolyte disturbances are more severe in HHS, and it carries a higher morbidity and mortality
The biochemical criteria for HHS diagnosis are:
- Serum glucose >33.3 mmol/L
- Venous pH >7.25 (or arterial pH >7.30) or bicarbonate >15 mmol/L
- Negative or small ketonuria, absent to mild ketonaemia
- Elevated serum osmolality >320 mOsm/kg*
- Anion gap may be variable#
*Serum osmolality = 2 x (sodium) + glucose + urea mmol/L
#Anion gap = serum sodium – (chloride + bicarbonate). Normal anion gap 4-13 mEq/L
Clinical overlap between HHS and DKA can make diagnosis challenging, but distinction between the two is essential in guiding management
Clues to diagnosis, distinguishing HHS from DKA, may include:
| Distinguishing HHS from DKA |
HHS
|
DKA
|
|
Serum glucose
|
Extremely high
|
High
|
|
Serum osmolality
|
>320 mOsm/kg
|
May be elevated in severe DKA
|
|
Serum pH
|
pH >7.25
|
pH
<7.3
|
|
Serum bicarb
|
HCO3 >15
|
HCO3
<15
|
|
Serum ketones
|
Ketones
<3 mmol/L
(may be mildly elevated if severely dehydrated)
|
Ketones >3 mmol/L
|
|
Onset
|
Days to weeks
|
Hours to days
|
|
Dehydration
|
Severe, often underestimated
|
May be overestimated
|
Precipitants and risk factors
- Obesity
- Undiagnosed or uncontrolled diabetes, especially type 2 diabetes
- Acute illness, stress or substance use
- Very high carbohydrate consumption
- Medications eg corticosteroids, atypical antipsychotics, phenytoin, beta-blockers
Assessment
History and examination are directed towards potential precipitants, assessment of severity and detection of HHS complications
History
- Polydipsia and/or polyuria
- Weight loss and/or increased appetite
- Lethargy, behaviour change or confusion
- Abdominal pain, nausea or vomiting
- Signs of underlying infection or precipitating illness
- Family history of type 2 diabetes
Examination
Assess dehydration
- Signs of severe dehydration may include shock (poor perfusion, rapid pulse or hypotension)
- Caution: dehydration is usually severe and under-recognised. Hyperosmolality maintains intravascular volume and masks clinical signs. Assume at least 12-15% fluid deficit
Assess neurological status
Look for signs of underlying infection or illness
Note: deep sighing respiration (Kussmaul breathing) is a sign of DKA
Management
Where possible, children and adolescents with HHS should be managed in a paediatric high dependency or intensive care unit
Investigations
Bloods
- Blood glucose
- Venous blood gas (VBG)
- Urea, creatinine and electrolytes (UEC) and calcium, magnesium and phosphate (CMP)
- Full blood count (FBC)
- Blood ketones (bedside test, normal
<0.6 mmol/L)
- Blood cultures if febrile or suspicion of sepsis
Urinary ketones
Consider ECG if potassium results will be delayed as hypokalaemia is common
Consider septic work up if clinically indicated. This may include blood culture, urine culture lumbar puncture and/or chest x-ray
Treatment
Goals of treatment
- Correct dehydration and restore circulating volume with fluid resuscitation
- Correct hyperosmolality with ongoing fluid therapy
- Correct hyperglycaemia – initially with fluid replacement alone, then with addition of insulin
- Correct electrolyte deficiencies
- Monitor for and treat complications (thrombosis, rhabdomyolysis, malignant hyperthermia)
- Identify and treat precipitating causes
Management of HHS
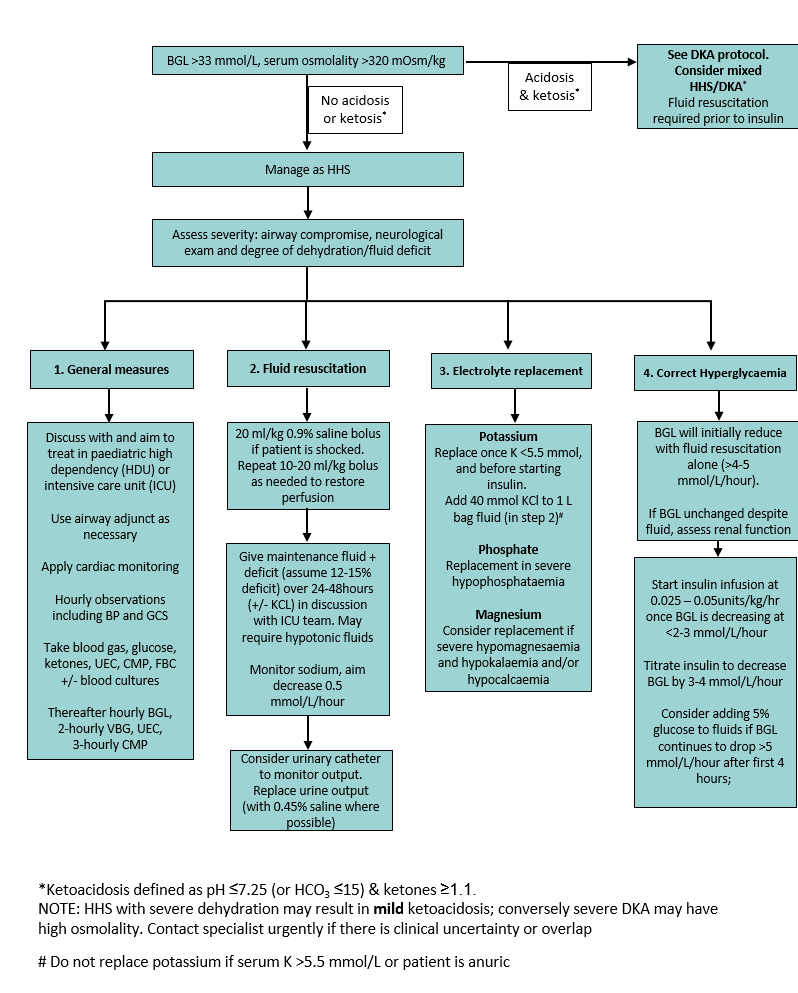
Fluid resuscitation
- If shocked, administer 10-20 mL/kg 0.9% sodium chloride IV bolus. Repeat if required to restore peripheral perfusion and discuss with senior clinician, intensive care unit (ICU) or retrieval team
- Deliver ongoing IV fluid as full maintenance fluids + estimated fluid deficit (typically 12-15%) over 24-48 hours
- The child will likely require hypotonic maintenance fluid (eg 0.45% sodium chloride) to reduce osmolality. This should only be done under guidance of an ICU/retrieval team
- If child has ongoing poor perfusion or is haemodynamically unstable, or where hypotonic fluids are unavailable, consider 0.9% sodium chloride maintenance fluid.
Isotonic fluid will improve intravascular volume, whilst hypotonic fluids will
prevent increasing serum osmolality
- Monitor and replace urine output (where possible, replace urine output with 0.45% sodium chloride, as urine will be hypotonic)
- Cease IV fluid once pH and bicarbonate have normalised and child is tolerating oral intake
Potassium
- Children with HHS have a deficit of total body potassium
- Maintain serum potassium between 4-5 mmol/L
- Do not replace potassium if patient is anuric or serum potassium is >5.5 mmol/L
- If insulin is commenced, check serum potassium within one 1 hour and 2-4 hourly thereafter. Higher rates of potassium replacement may be required
- ECG and cardiac monitoring are required to recognise early signs of potassium derangement
Sodium
- Measured sodium is depressed by the dilutional effect of hyperglycaemia
- Corrected sodium can be calculated as:
Corrected sodium = measured sodium + 0.3 x (glucose – 5.5) mmol/L - Sodium may initially rise with fluid resuscitation. This is due to the correction of hyperglycaemia and decrease in osmolality, which allows water to re-equilibrate with dehydrated cells, as well as ongoing water loss in urine. Thereafter sodium levels
will fall as fluid is replaced
- Aim for a decrease in sodium of 0.5 mmol/L/hour
- If sodium does not rise as the glucose falls during initial treatment, or if hyponatraemia develops, this may indicate excessive fluid correction and increases risk of cerebral oedema
Glucose
- Only administer insulin following adequate fluid resuscitation and rehydration
- Blood glucose level (BGL) should initially fall with adequate rehydration alone (initially 4-5 mmol/hour, and gradually slowing). A more rapid fall in BGL and osmolality may decrease intravascular volume and lead to circulatory collapse
- Start IV insulin infusion when BGL decreases at a rate
<2-3 mmol/L/hour with fluids alone
- Insulin infusion is lower in HHS than in DKA, due to relative insulin sufficiency and less ketosis
- Do not give subcutaneous insulin or insulin bolus
- Insulin infusion can be run as a sideline with the rehydration fluids via three-way tap provided a syringe pump is used
- Failure of expected fall in glucose should prompt reassessment of renal function
- Following recovery many children with type 2 diabetes and HHS will require insulin treatment only temporarily, and many can be managed effectively with diet and oral agents ongoing
Phosphate
- Severe hypophosphataemia may increase risk of rhabdomyolysis
- Consider replacing phosphate in preparations that contain potassium, to replace phosphate and potassium simultaneously (monitor potassium levels hourly during replacement)
Magnesium
- Significant hypomagnesaemia may contribute to hypocalcaemia, but often does not need replacement
- Consider magnesium replacement in severe cases and monitor serum magnesium levels
Complications of HHS
The most important complications of HHS are
- Venous thrombosis, especially with central venous catheters
- Rhabdomyolysis
- Malignant hyperthermia
- Compartment syndrome
- Cerebral oedema, may result from rapid correction of hyperglycaemia/hyperosmolality
- Ventricular arrhythmias, secondary to electrolyte disturbance
Consider consultation with local paediatric team for
- All children with HHS
- All children with newly diagnosed diabetes mellitus
Consider transfer when
- Child requiring care above the level of comfort of the local hospital
- Children and adolescents with HHS should be managed in a unit that has:
- Access to laboratory services for frequent and timely evaluation of biochemical variables
- Paediatric high dependency or intensive care unit
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Last updated July 2024