See also
Online paediatric BP centile calculator
BP by age and height centile tables: boys girls
Key points
- Severe hypertension requires urgent consultation and management. Hypertension associated with encephalopathy is a medical emergency
- All hypertension in children requires monitoring and follow-up
- Blood pressure should be measured annually in healthy children
- Where possible, abnormal machine BP measurement should be confirmed, preferably with a manual BP, ensuring appropriately sized cuff is used for accurate measurement
Background
- This guideline will focus on the paediatric population aged 1–17 years (not infants)
- Hypertension in childhood is a key predictor of risk for hypertension, cardiovascular disease and end organ damage in adulthood
- Primary/essential hypertension accounts for the majority of hypertension in children >6 years old and is generally associated with obesity or a family history of hypertension
- Secondary hypertension is more common in younger children (<6 years old) with renal disease being the most prevalent cause. This population is at greater risk of hypertensive emergencies due to an underlying condition
Assessment
Risk factors
- Overweight/obesity
- Male sex
- Family history of hypertension
- Low birth weight/intrauterine growth restriction
- Prematurity
- Excess dietary salt intake
- Physical inactivity
- Chronic health concerns, eg chronic kidney disease, diabetes
|
Causes of Hypertension |
|
Primary Hypertension |
|
Situational Hypertension |
|
Stress, pain, anxiety |
|
Secondary Hypertension |
|
Renal parenchymal disease |
GN, polycystic kidneys, CKI |
|
Cardiac, Vascular |
Renal artery stenosis, Coarctation repair (pre and post) |
|
Endocrine |
Diabetes, thyroid disease, CAH, Diabetes, thyroid disease, CAH, Cushings |
|
Autoimmune |
Thrombotic thrombocytopenic purpura, Haemolytic Uraemic Syndrome,
Henoch-Schönlein Purpura |
|
Genetic/Syndromic |
Neurofibromatosis, Williams Syndrome, Turners Syndrome |
|
Malignancy |
Wilms tumour, neuroblastoma, pheochromocytoma |
|
Intracranial pathology |
Intracranial haemorrhage/stroke, pituitary adenoma, raised ICP |
|
Respiratory |
Chronic lung disease, OSA |
|
Drug-induced |
Corticosteroids, OCP, stimulants |
History
- Headache/vomiting
- Blurred vision
- Change in mental state
- Seizures
- Chest pain/palpitations
- Shortness of breath
- Cardiac failure
- Past history of Acute Kidney Injury (AKI)
Examination
- Confirm hypertension (See measuring blood pressure section below)
- Vitals: tachycardia, four limb BP for upper and lower limb discrepancy
- Height and weight: obesity, growth retardation
- Signs of end organ damage
- Fundoscopy: hypertensive retinopathy
- Cardiovascular: apical heave, hepatomegaly, oedema
- Chronic renal failure: palpable kidneys
- Focal neurology eg facial nerve palsies
- Signs of underlying cause
- General appearance: Cushingoid, proptosis, goitre, webbed neck (Turner syndrome), elfin facies (William syndrome)
- Skin: Cafe-au-lait spots, neurofibromas, acanthosis nigricans, hirsutism, striae, acne, rash (vasculitis)
- Cardiovascular: murmurs +/- radiation, apical heave, reduced femoral pulses, oedema, hepatomegaly (CCF)
- Abdomen: masses, palpable kidneys, flank bruits
- Genitourinary: ambiguous/virilised genitalia eg CAH
Key points when measuring blood pressure
(See video)
Ensure the correct cuff size is selected for each patient, favouring a larger rather than smaller cuff (smaller cuff creates artificial hypertension)
- BP cuff width should be 40% of the length of the arm measure from the shoulder tip to the elbow
- Abnormal oscillatory BP measurement needs checking with a manual BP from the child's arm
The table below identifies BP levels requiring further evaluation, starting with repeating the BP manually ensuring accurate measurement
|
*Screening BP Values Requiring Further Evaluation |
|
Age (years) |
Blood pressure (mmHg) |
|
|
Boys |
Girls |
|
|
Systolic |
Diastolic |
Systolic |
Diastolic |
|
1 |
98 |
52 |
98 |
54 |
|
2 |
100 |
55 |
101 |
58 |
|
3 |
101 |
58 |
102 |
60 |
|
4 |
102 |
60 |
103 |
62 |
|
5 |
103 |
63 |
104 |
64 |
|
6 |
105 |
66 |
105 |
67 |
|
7 |
106 |
68 |
106 |
68 |
|
8 |
107 |
69 |
107 |
69 |
|
9 |
107 |
70 |
108 |
71 |
|
10 |
108 |
72 |
109 |
72 |
|
11 |
110 |
74 |
111 |
74 |
|
12 |
113 |
75 |
114 |
75 |
|
≥13 |
120 |
80 |
120 |
80 |
*90th centile for a child at average height
Assessment of severity
Interpreting blood pressure measurement
An
online blood pressure centile calculator specific for gender, age and height can be used to determine the severity of hypertension
|
Blood pressure classification in children and adolescents |
|
|
For children aged 1 to 13 years |
For children aged 13-17 years |
|
Normal blood pressure |
<90th centile |
<120/<80 mmHg |
|
Elevated blood pressure |
≥90th centile to
<95th centile or 120/80
mmHg to
<95th centile (whichever is lower) |
120/<80 to 129/<80 mmHg |
|
Stage 1 Hypertension |
≥95th centile to
<95th centile + 12 mmHg or 130/80 to 139/89 mmHg (whichever is lower) |
130/80 to 139/89 mmHg |
|
Stage 2 Hypertension |
≥95th centile + 12 mmHg, or ≥140/90 mmHg (whichever is lower) |
≥140/90 mmHg |
|
Severe Hypertension |
|
Hypertensive Urgency |
>95th centile + 30 mmHg without symptoms/signs of target end organ damage (See Examination) |
>180/120
without symptoms/signs of target end organ damage (See Examination) |
|
Hypertensive Emergency |
>95th centile + 30 mmHg associated with encephalopathy,
eg headache vomiting, vision changes and neurological symptoms (facial nerve palsy, lethargy, seizures, coma) +/- target-end organ damage |
>180/120
associated with encephalopathy,
eg headache vomiting, vision changes and neurological symptoms (facial nerve palsy, lethargy, seizures, coma) +/- target-end organ damage |
Management
Emergency management of severe hypertension
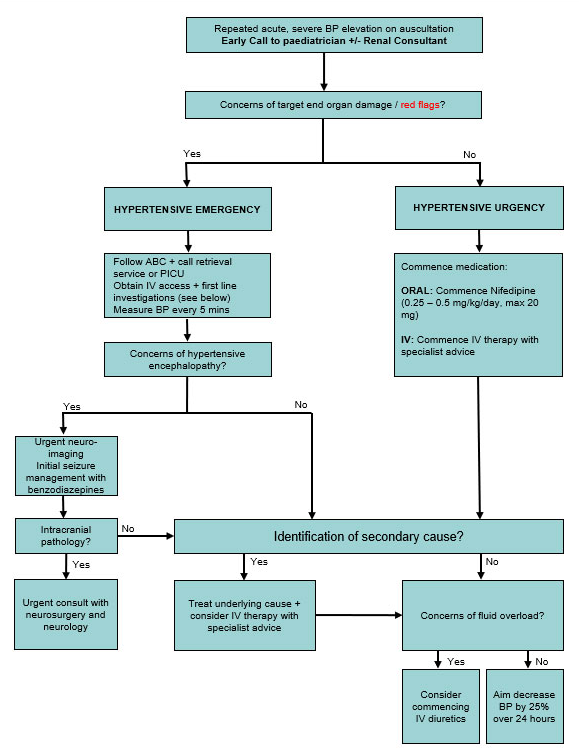
- Discuss with renal team and retrieval/ICU team
Hypertensive urgency
If medically stable, consider short acting oral agents while investigating cause
- Nifedipine
- Commence 0.25–0.5 mg/kg/day (max 20 mg) and titrate up as required to a maximum of 3 mg/kg/day (max 120 mg)
Hypertensive emergency
- Intravenous therapy; discuss with renal team and retrieval/ICU team
- Aim to gradually reduce BP to the patient's estimated 95th centile
- Decrease BP by 25% of the original value every 24 hours till target BP reached. Reduce rate of decrease if patient becomes symptomatic
Hypertension without severe features
Investigations
First-line investigations
- UEC, CMP, urinalysis +/- renal ultrasound
- Consider LFT, Hb1Ac, fasting lipids particularly in children with BMI >95th centile
Further investigations should only be considered in consultation with a general or renal paediatrician
Consider further testing if child meets one of the following criteria:
-
<6 years
- Concerns for secondary causes on history/examination
- Abnormal first-line investigations
Further Investigations
- Bloods: FBE, Bicarbonate, renin/aldosterone ratio, TFT, plasma metanephrins, cortisol, fasting glucose
- Urine: microscopy, protein/creatinine ratio, catecholamines, drug screen
- Imaging: renal doppler ultrasound, DMSA, CTA/MRA
- Other: echocardiogram, sleep study
Lifestyle counselling
Dietary modifications
- Rich in fresh fruit and vegetables/legumes, fish, poultry, lean red meat and low fat dairy
- Limit intake of high sodium, fat or sugar containing foods
Lifestyle modifications
- Increase physical activity, aiming 40 minutes moderate to vigorous exercise 3-5 days/week
- Consider counselling/behavioural techniques to help address weight management and metabolic risk
Medical management
Should be commenced if:
- Conservative measures have failed
- Symptomatic hypertension develops
- Stage 2 hypertension with no modifiable risk factors
- Hypertension in setting of chronic kidney disease/diabetes
Medical management should only be commenced in consultation with a general or renal paediatrician
- Long-acting calcium channel blockers such as amlodipine are recommended as first line therapy. Other medication may be preferred in children with BMI >95th centile, diabetes or proteinuria
Consider consultation with local paediatric team when
- Red flags (see history section above) or ongoing concerns are present
- Hypertensive urgency or hypertensive emergency
- Medical management of hypertension is required
Consider transfer when
Child requiring care beyond the comfort level of the hospital
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
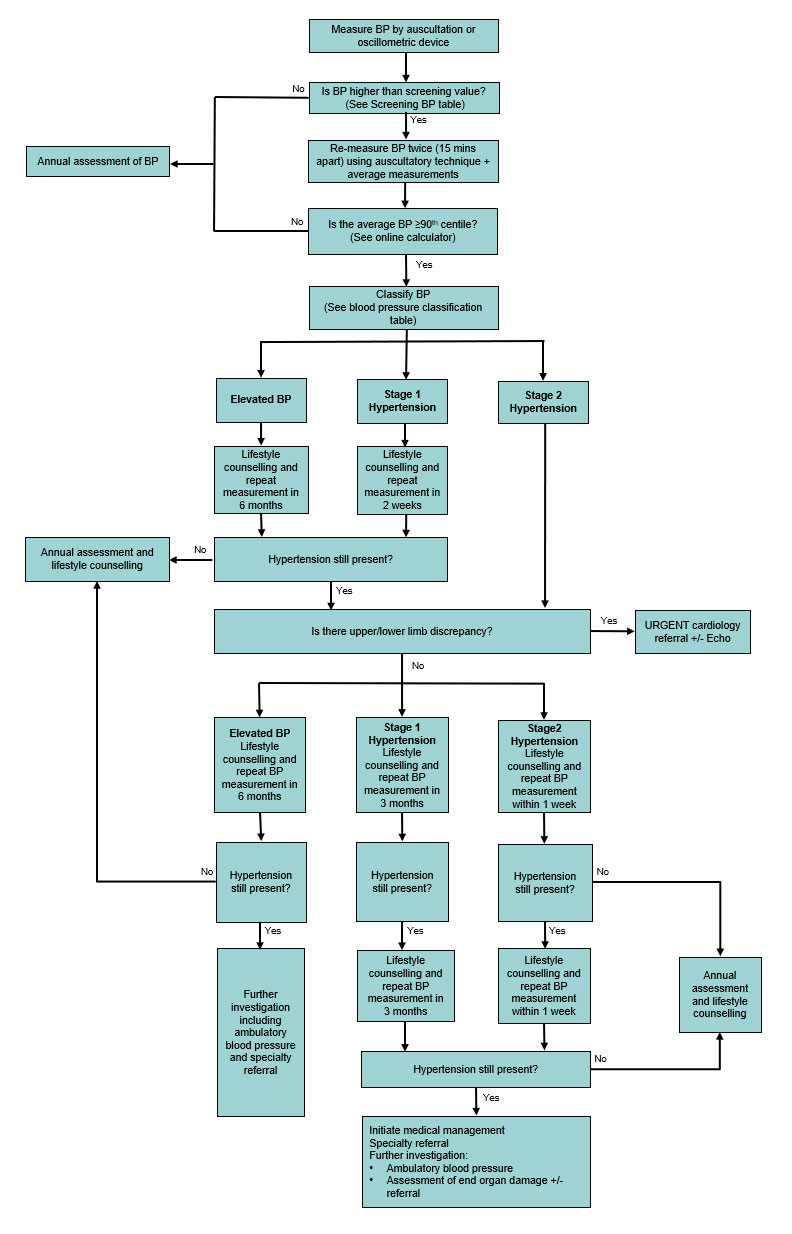
Hypertensive children without severe features may be discharged with appropriate follow-up (See flowchart)
Parent information
See
Parent resources
Additional notes
How to Measure Blood Pressure – American Academy of Pediatrics (video)
Last updated June 2021