See also
Pneumonia
Sepsis
Febrile Child
Key points
- Consider the presence of a parapneumonic effusion in an unwell child with pneumonia or a child with pneumonia who has persistent fever despite 48 hrs of appropriate antibiotic treatment
- The stage of the effusion determines the likely treatment. A simple effusion may resolve with antibiotics, while a more organised or complicated effusion will likely require pleural space drainage
- A well child with a simple effusion may be managed as an outpatient
- An unwell child with a complicated effusion should be referred to the respiratory and/or surgical teams for consideration of drainage
Background
- A pleural effusion is a pathological collection of fluid between the parietal and visceral pleura
- A parapneumonic effusion is a pleural effusion associated with adjacent pneumonia
- A simple parapneumonic effusion is a non loculated transudate which is sterile
- A complicated parapneumonic effusion is a loculated effusion or empyema, with changes in the pleural fluid due to bacterial invasion of the pleural space
- Streptococcus pneumoniae, Staphylococcus aureus and Group A Streptococcus are the most common causes of an empyema
Assessment
History
- Fever
- Particularly fever that persists after 48 hours of appropriate treatment of pneumonia
- Tachypnoea
- Cough
- Increased work of breathing/respiratory distress
- Pleuritic chest pain or abdominal pain
Examination
- Appears lethargic/unwell
- Hypoxaemia
- Tachypnoea
- Chest wall in-drawing, splinting, retractions, grunting, nasal flaring
- Bronchial breath sounds and crackles (adjacent pneumonia)
- Localised absence of breath sounds and a dull percussion note
Assessment of severity
Severity depends primarily on the clinical status of the child and may not correlate with the size or appearance of the effusion
- Severe respiratory distress
- Severe hypoxaemia or cyanosis
- Marked tachycardia
- Altered mental state
Differential diagnosis
The majority of pleural effusions are secondary to bacterial pneumonia. Other less common causes include:
- Atypical infection (tuberculosis, mycoplasma)
- Malignancy
- Foreign body
- Congestive cardiac failure
- Serositis from rheumatological causes
Management
Investigations
No laboratory tests are diagnostic, but consider the following:
Bloods
- FBE
- UEC (consider SIADH and atypical HUS)
- CRP (useful marker of treatment success)
- Blood culture
- LFTs (albumin) and coagulation studies may be indicated for severely unwell children (consider toxic shock syndrome)
Specific tests
- Viral swabs including COVID-19 and influenza
- Pneumococcal PCR (blood)
- Testing for mycobacterium tuberculosis, consult with local infectious diseases team
If inserting a drain, consider sending pleural fluid for
- Gram stain, MC&S
- Pneumococcal PCR
Chest imaging
- Anteroposterior CXR
- Chest ultrasound: Can distinguish between a simple or complicated effusion
- Chest CT is not routinely recommended. It may be considered in cases where the child fails to respond to treatment or suspecting alternate aetiology (malignancy, foreign body)
Treatment
A child with a small simple effusion and no respiratory distress, who can tolerate oral antibiotics can be managed as an outpatient (see
Pneumonia)
Admission to hospital is required for respiratory support (hypoxia, moderate to severe work of breathing), hydration support, IV antibiotics and for investigations to assess the severity of the effusion
Supportive care
- Provide supplemental oxygen if required
- If giving NG or IV fluids as maintenance, limit to 2/3rds of child’s calculated fluid requirement to avoid fluid overload, with regular clinical review of fluid status
- Analgesia
- Encourage mobilisation
Antibiotics
- Antimicrobial recommendations may vary according to local antimicrobial susceptibility patterns; please refer to
local guidelines
- Suggest 3rd generation cephalosporin as first line
- Consider staphylococcal MSSA and MRSA coverage
- Definitive management should be based on investigation results and local specialist advice
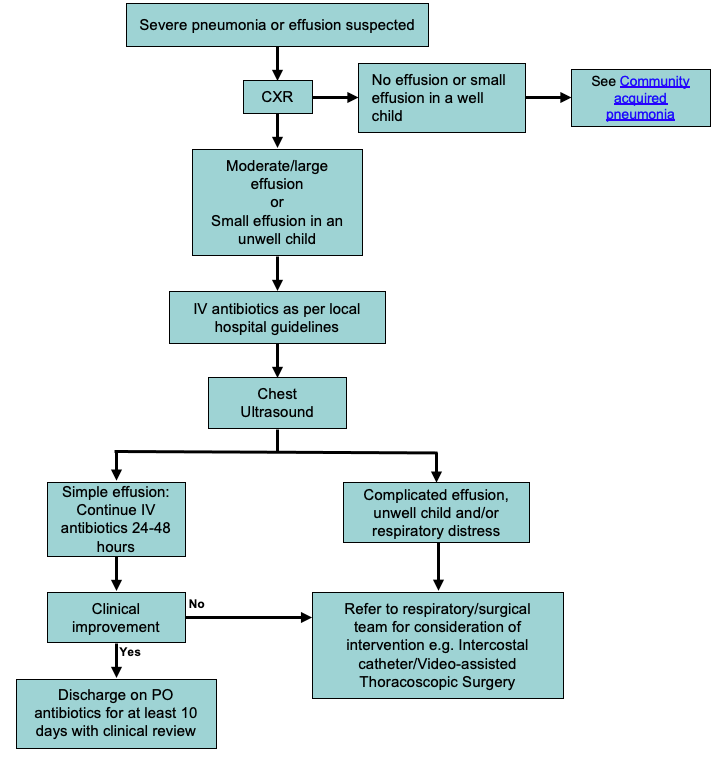
Management of suspected parapneumonic effusion
Consider consultation with local paediatric team when
Any child with pleural effusion requiring admission
Consider consultation with respiratory and/or surgical team when
Any child with:
- A complicated effusion
- Severe respiratory distress
- Septic shock (drain may be required for source control)
- Ongoing fever and/or respiratory distress after 48hrs of IV antimicrobials
Consider transfer when
Any child with:
- A complicated effusion where surgical intervention is anticipated
- Comorbidities such as cardiac disease, chronic respiratory disease, immunodeficiency or immunosuppression
- High level respiratory support required
A child requiring care beyond the comfort level of local hospital
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Consider discharge when
The child is:
- Tolerating oral antibiotics
- Afebrile
- Not requiring supplemental oxygen
- Tolerating adequate oral intake
Last updated August 2022