See also
Acute asthma
Asthma in adolescents (12 years and over)
Asthma in primary school-aged children (6-11 years)
Bronchiolitis
Key points
- This guideline provides advice for diagnosing and managing preschool aged children with asthma. See Acute asthma for acute management
- Most preschool aged children have infrequent mild episodes of wheeze that are triggered by respiratory viruses and do not require a preventer
- A therapeutic trial of short-acting beta agonist (SABA) or inhaled corticosteroid (ICS) may be needed to help diagnose asthma in a preschool aged child
- First-line preventer treatment for preschool aged children with asthma is low dose ICS with spacer, titrated according to response. Many children will grow out of asthma prior to primary school
- Additional management includes regular asthma education, reviewing inhaler technique and annual influenza vaccine
Background
This guideline defines preschool asthma as children between 1-5 years old who present with recurrent episodes of wheeze, cough or difficulty breathing/activity limitation, all of which respond to SABA
- The diagnosis of asthma in preschool aged children can be difficult as there is overlap with other common conditions and a lack of objective tests
- Wheeze in children <1 year is most likely caused by bronchiolitis
- Currently there are no valid ways of sub-typing children with preschool wheeze/asthma. Previously used classification systems, such as viral induced episodic wheeze and multi-trigger wheeze have been shown to have poor clinical performance and should not be used
Most preschool aged children have infrequent mild episodes of wheeze (>6 weeks between episodes) that are triggered by respiratory viruses and do not require a preventer
- The focus should be on adequate symptom control and regular titration of asthma treatment to ensure this is achieved
- Asthma medications and delivery devices include:
- Inhaled corticosteroid (ICS)
- Short-acting β-agonist (SABA)
- Long-acting β-agonist (LABA)
- Metered dose inhaler (MDI)
A diagnosis of asthma in the preschool years does not mean the child will have asthma forever. Only half of children who wheeze during preschool years will have asthma at school age
Assessment
History
Features of preschool asthma
- Recurrent episodes of wheeze (2 or more)
- Cough
- Difficulty breathing (characterised by activity limitation)
- All of which respond to asthma treatment (SABA and/or regular ICS)
Additional Features
- Interval symptoms
- Daytime symptoms
- Need for reliever/SABA (number of doses per week)
- Activity limitation
- Symptoms at night or on waking
- Need for systemic corticosteroid, ED presentation or hospital admission for asthma treatment
- Previous ICS use
- Inhaler technique
Examination
- Wheeze, signs of airflow obstruction (prolonged expiratory phase, intercostal recession, subcostal recession)
- Look for signs of comorbidity, including allergic rhinitis and eczema
- Measure height and weight at least annually in those on ICS, ideally measure every 3-6 months
- Review inhaler technique
Management
Investigations
- No investigations are routinely required
- Chest X-rays are not required
- Lung function tests cannot be used in preschool aged child
Treatment
Preferably recurrent symptoms and signs of asthma AND response to SABA is observed and documented by a health professional
Refer to flowchart below for children with a history of recurrent wheeze, cough or SOB (can be based on caregiver report alone)
Approach to children with history of recurrent wheeze, cough or SOB
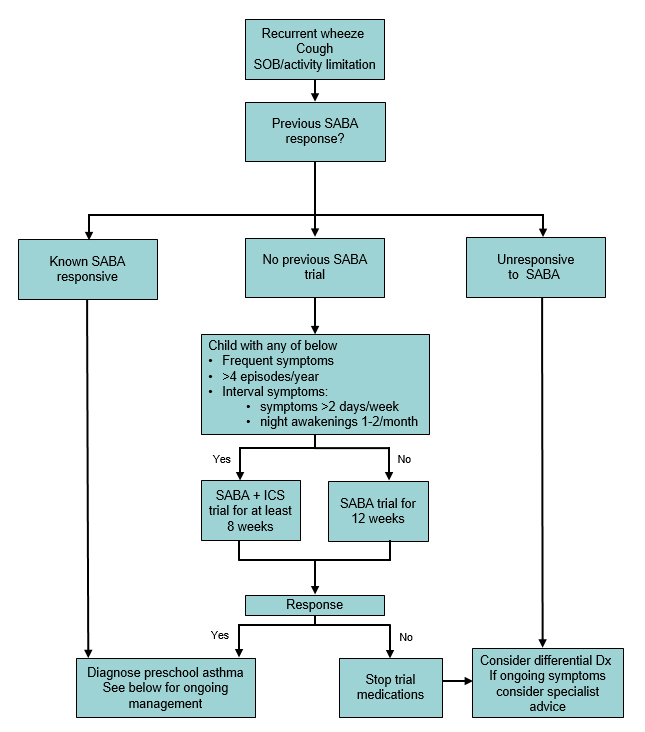
Diagnosis and treatment response should be reviewed and re-evaluated 8-12 weeks after initial prescription
- If stable, trial off preventer treatment and reassess control in 3 months’ time
- Stop the medication if there is no benefit after the trial
- See diagram below on Step approach in maintenance treatment
Inhaler Devices
Preschool age children should be prescribed MDI with a spacer and facemask until they are coordinated enough to use the mouthpiece (often around 4 years old)
See videos demonstrating correct inhaler technique
Reliever treatment
All children should be prescribed SABA with spacer and encouraged to always have spacer with them
Dose: salbutamol 100mcg MDI, up to 6 puffs (via spacer +/- mask)
Maintenance treatment (preventer)
Indications for commencing preventer treatment are
- Frequent daytime symptoms (2 or more times a week)
- Frequent night-time symptoms (2 or more times a month)
- Recurrent hospital presentations requiring asthma treatment (2 or more in one year)
- Frequent exacerbations (4 or more episodes per year)
First line preventer treatment is low dose ICS
- Dose: fluticasone proprionate 50mcg 1 BD
Montelukast oral tablet can be used as an alternative first line preventer (or adjunct to ICS) in children requiring further control
- Dose: montelukast 4mg once daily (5mg if >5 years old)
- Consider using as ICS alternative if significant parental concern regarding steroids or in children where use of MDI + spacer is particularly difficult
- 1 in 6 children may develop side effects with this medication including agitation, sleep disturbance and altered mood. If this occurs, cease medication to see if symptoms resolve
Combination ICS/LABA inhalers are not recommended in this age group outside of specialist use
Step approach in maintenance treatment
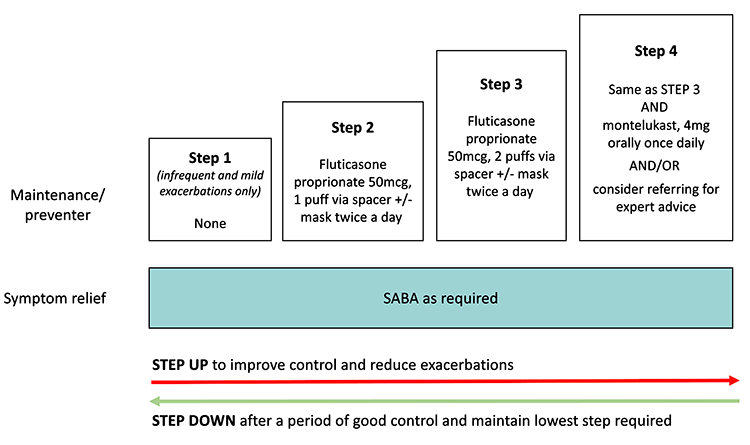
Adapted from Australian Asthma Handbook, GINA and McNamara
Stepping up or down according to response
The degree of symptom control, irrespective of the current regimen, informs whether changes need to be made to the preventer treatment
|
Good control
(All of) |
Partial control
(One or two of) |
Poor control
(Three or more of) |
Daytime symptoms |
≤2 days per week |
>2 days per week |
>2 days per week |
Need for reliever* |
≤2 days per week |
>2 days per week |
>2 days per week |
Limitation to activity |
none |
present |
present |
Night-time symptoms (or on waking) |
none |
present |
present |
* Reliever frequency does not include doses taken prophylactically before exercise
Review asthma control in 6-12 weeks:
- If poorly controlled:
- Always check correct technique and adherence prior to stepping up
- Consider alternate diagnoses
- Consider step up if indicated
- Good control for approximately 3 months suggests preventer treatment could be stepped down
- Continue the lowest treatment that controls symptoms
- Only cease treatment after a period of 3 months symptom-free and review 4-6 weeks after stepping down
- Consider ongoing management of triggers and seasonal factors when stepping treatment up or down
Education
- Assess knowledge and understanding and address gaps on
- symptom recognition and management
- when to seek medical attention
- emergency management
- role of reliever and preventer treatment
- inhaler technique
- Recommend annual influenza vaccine
- Check adherence at every visit and address barriers
- Asthma Action Plan: all children should have a written action plan for at home and childcare
Management of acute exacerbations in the community
- See Acute asthma
- In children already taking daily ICS, there is no role for increasing the dose of ICS during an exacerbation
- Prednisolone should not be prescribed for preschool asthma outside of the Emergency Department or hospital setting (unless an exacerbation is being managed in a general practice and a transfer to emergency is being arranged)
Approach to asthma not responding to treatment
Consider consultation with local paediatric team, respiratory or specialist asthma service when
- Inadequate asthma control achieved at Step 4
- Diagnosis of asthma uncertain
For emergency advice and paediatric or neonatal ICU transfers, see Retrieval Services
Parent information
Asthma Australia: Asthma in preschool aged children
RCH Kids Health Info: Asthma Videos
Additional resources
Asthma Handbook: Resources
Asthma Handbook: Asthma Action Plans for adults and adolescents
Asthma action plan library
Green prescribing
Breathe Green Project
Last updated June 2023