See also
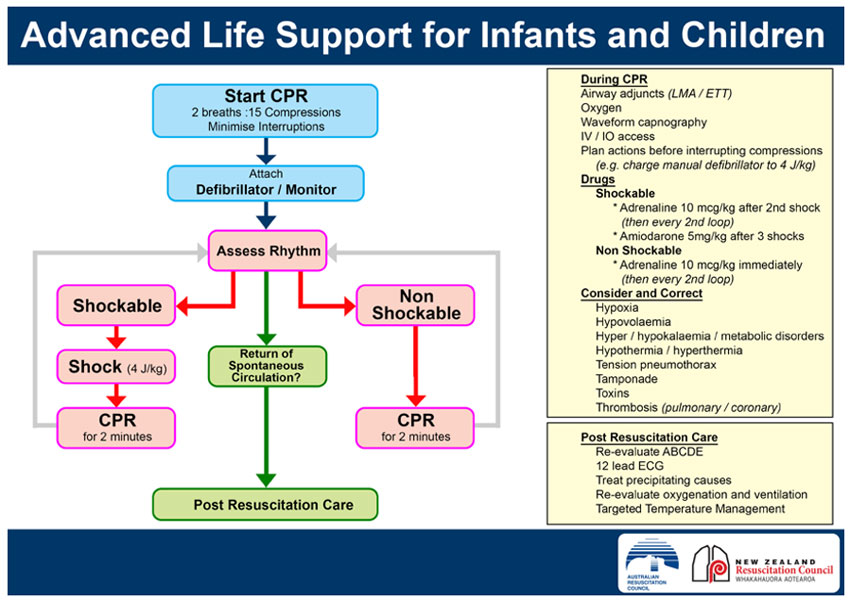
APLS algorithms
Resuscitation: hospital management of cardiopulmonary arrest COVID-19
Resuscitation: care of the seriously unwell child
Recognition of the seriously unwell neonate and young infant
Key points
- Cardiac arrest should be suspected in an infant or child who is unresponsive and not breathing normally — pulse check should not delay cardiopulmonary resuscitation (CPR)
- CPR should be commenced if cardiac arrest is suspected
- Ongoing management should be directed by the cardiac rhythm identified
- Effective resuscitation relies on a coordinated team and good communication
Background
- The majority of arrests in children are due to hypoxia, hypotension and acidosis
- The most common dysrhythmias are severe bradycardia and asystole
- Ventricular fibrillation (VF) is the initial arrest rhythm in approximately 10%
- Traumatic cardiac arrest is a unique situation - the management is different to non-traumatic cardiac arrest and is not covered by this CPG
- Early allocation of roles can optimise resuscitation (if personnel available)
- Team leader
- Airway nurse and doctor
- Circulation nurse and doctor
- Cardiac compression personnel
- Defibrillator operator
- Assessment doctor
- Scribe + time keeper with stop watch
Resuscitation
Assess for signs of life or response; if they are absent commence CPR
A – Airway
Look, listen, feel for patency/added noises
Optimise head position
Consider simple airway manoeuvres (head-tilt chin-lift or jaw thrust)
Suction secretions/blood/vomit
B – Breathing
Look for chest rise and fall and auscultate
Commence artificial ventilation with self-inflating bag-valve-mask or anaesthetic t-piece using 100% oxygen
Consider oro/nasopharyngeal airway for upper airway obstruction
Consider 2-person technique for poor mask seal
Intubation should be considered for persistent obstructed airway or at some stage during CPR (see Emergency airway management)
*If available, continuous wave-form end-tidal CO2 monitoring, should be used to:
- Warn of accidental extubation during CPR
- Monitor for return of spontaneous circulation
- Ensure adequacy of ventilation
C - Circulation
If no signs of life continue CPR
If signs of life assess pulse
Palpate central pulse (brachial, femoral, carotid)
Assessment of pulse can be difficult and inaccurate
If no pulse, slow pulse (<60 in an infant) or unsure, continue CPR
Determine the cardiac rhythm: shockable or non-shockable
(see Advanced Life Support flow chart above)
Technique
External cardiac compression
- CPR rate for all ages 100–120 bpm
- Ratio for CPR is 2 breaths : 15 compressions
- Once patient intubated compressions and breaths are independent of each other: compressions continue at rate 100–120 bpm and breaths at rate of 10 bpm
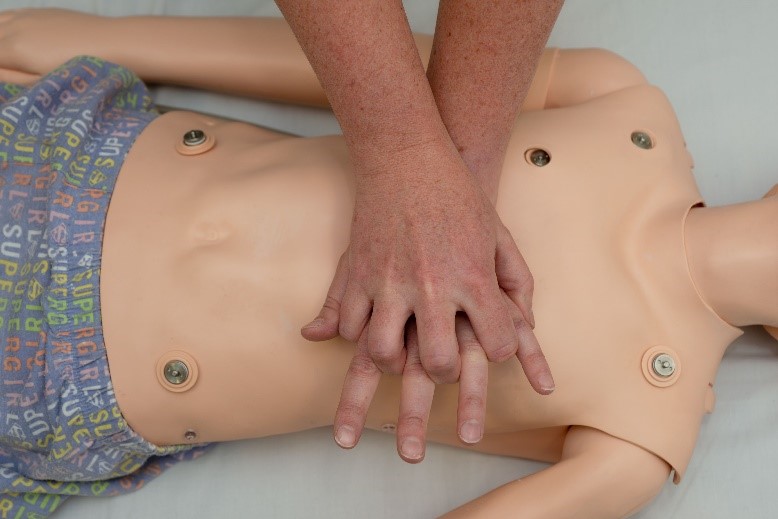
- Place the child on a firm surface. If on a bed, place the cardiac compression board under the patient, not under the mattress
- Perform external cardiac compressions to the lower half of the sternum in all patients including newborns
- Compress sternum 1/3 the depth of the chest
- Use the hand technique that allows you to achieve this:
For newborn infants the best technique is a two-handed hold in which both thumbs compress the sternum

For infants two fingers may be used

For small children use the heel of one hand

For larger children use the "heel" of one hand with the other superimposed
DO NOT interrupt CPR except for rhythm check or defibrillation
Defibrillator operator instructions:
"HANDS OFF” – pad placement or DC shock – “Continue CPR" – “HANDS ON”
For rhythm check consider “COACHED”
Continue CPR
Oxygen away
All clear
Charge
Hands off
Evaluate rhythm
Defibrillate or ‘dump charge’
- Frequent changes of cardiac compression personnel (every few minutes) is desirable
- Continue CPR until the next designated rhythm check
- Gain IV access as soon as possible
- Consider
intraosseous access early
- If DC shock delivered, recommence CPR immediately for 2 minutes prior to rhythm check
During resuscitation
Correct treatable causes
- Hypoxaemia
- Hypovolaemia
- Hypo/hyperthermia
- Hypo/hyperkalaemia
- Tamponade
- Tension pneumothorax
- Toxins/poisons/drugs
- Thrombosis
Other considerations during resuscitation
- Aim for normal glucose
- Aim for normal carbon dioxide (CO2)
- Aim for normal temperature
- Toxin induced cardiac arrest requires urgent consultation with National Poisons Centre 13 11 26
- Resuscitation for toxin induced cardiac arrest and cardiac arrest following cold-water drowning may be prolonged
Medications for paediatric arrest
Emergency Drug and Fluid Calculator
Monash Book drug doses
|
Drug |
Dose |
Indication |
|
Adrenaline 1:10,000 |
10 microgram/kg =
0.1 mL/kg IV/IM/IO |
Shockable and non-shockable cardiac arrest path
Non vagus-induced bradycardia |
|
Amiodarone |
5 mg/kg IV/IO |
Shock resistant ventricular fibrillation or pulseless ventricular tachycardia |
Atropine, lidocaine, sodium bicarbonate and calcium are only considered in specific situations
Extracorporeal Cardiopulmonary Resuscitation (ECPR)
ECPR is a procedure offered by specialised paediatric intensive care centres in Australia — eligibility should be discussed urgently with local retrieval service
Post resuscitation care - following return of spontaneous circulation
- Re-evaluate ABCD
- Ensure airway and breathing are managed effectively, including intubation if not already performed; do not extubate
- Titrate inspired to achieve normal saturations, avoid excessive oxygenation
- Ventilate to normal CO2
- Perform CXR to confirm ETT in desired position and check for complications of CPR (pneumothorax, rib fractures, aspiration)
- Maintain normal blood pressure appropriate for age with use of inotropes as needed
- Perform 12 lead ECG
- Monitor for further arrhythmias and consider ongoing anti-arrhythmic medication
- Consider echocardiography to monitor contractility and exclude tamponade
- Check haemoglobin, pH, electrolytes and glucose and correct as necessary
- Aim for normal temperature (avoid hypo/hyperthermia)
- Use adequate sedation and analgesia
Withdrawal of CPR
The decision to withdraw CPR in children is difficult and must involve experienced senior clinicians who will consider the clinical context and the desires of patient and family
Family and staff support
Family members of patients undergoing resuscitation should be given the option to be present, ideally with an assigned support person. Most hospitals are likely to have a family presence policy and staff education strategy in place.
Regardless of the outcome, resuscitation is stressful and can be psychologically traumatic to team members providing care. Debriefing and support should be offered to all involved staff who wish to attend
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Additional notes
ID badge size Resuscitation Card
Last updated May 2020