See also
Antibiotics
Febrile child
Febrile neutropenia
Emergency drug and fluid calculator
Invasive group A streptococcal infections: management of household contacts
Key points
- Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection
- It is important to diagnose sepsis quickly but also to not over-diagnose. Most children with fever (with or without a focus) do not have
sepsis (see assessment section below)
- Septic shock is sepsis with evidence of cardiovascular organ dysfunction; hypotension is a late sign
- Rapid vascular access, early initiation of empiric antibiotics and carefully titrated fluid resuscitation is vital
- Inotropes and vasopressors may be safely administered via peripheral cannula or intraosseous access (IO) in children during initial resuscitation
Background
- Sepsis is a major cause of morbidity and mortality in children
- Care delivered in the first hour following sepsis identification is crucial
High risk groups include:
- neonates
- immunocompromised children
- children with central venous access devices
- Aboriginal and Torres Strait Islanders
Major pathogens in infants
<2 months of age:
- Escherichia coli
- Group B Streptococcus
- Listeria monocytogenes is uncommon
- HSV infection should be considered in differential diagnosis of sepsis
Major pathogens in older children:
- Neisseria meningitidis
- Streptococcus pneumoniae
- Staphylococcus aureus (MSSA or MRSA)
- Group A Streptococcus (GAS)
Assessment
Sepsis or septic shock should be considered in a patient with a suspected or proven bacterial infection and any of the following
- Altered conscious state (lethargy, irritability, floppiness, weak cry)
- Unwell appearance ± non-blanching rash
- Features of cardiovascular dysfunction:
- reduced peripheral perfusion, pale, cool or mottled skin, prolonged central capillary refill time (CRT >2), tachycardia, decreased urine output (<1 mL/kg/hr) or narrow pulse pressure
- cold shock: narrow pulse pressure, prolonged capillary refill (more common in neonates/infants)
- warm shock: wide pulse pressure, bounding pulses, flushed skin with rapid capillary refill (more common in older children/adolescents and often under-recognised)
- Tachypnoea ± hypoxia ± grunting (not adequately explained by a respiratory illness)
- Unexplained pain
- Fever or hypothermia (temperature may be normal in neonates or the immunocompromised)
Toxin mediated sepsis: caused by superantigens from toxin-producing strains of S. aureus or GAS
- Clinical features may include fever, vomiting, diarrhoea, myalgia, conjunctival injection, confusion, collapse and a widespread erythematous rash
Red flag features
- High level of parental concern
- Representation within 48 hours
- Clinical deterioration despite treatment
- Recent surgery or burns
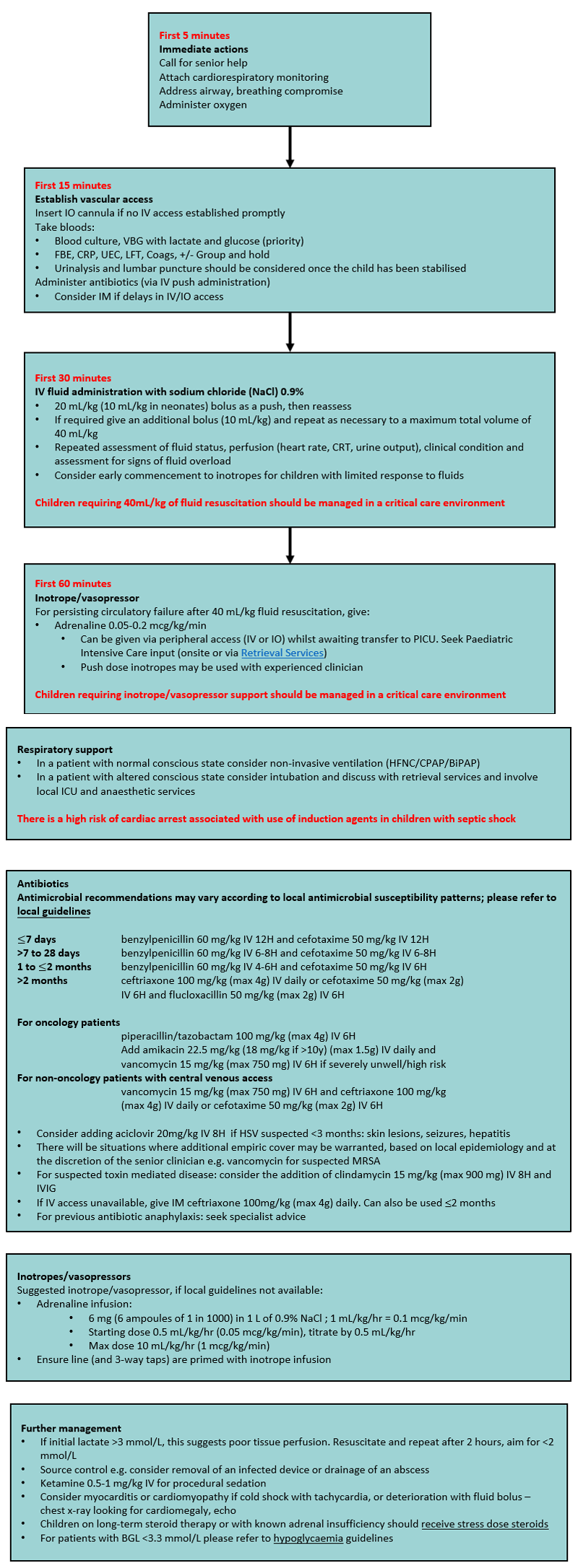
Management
Key principles in managing severe sepsis or septic shock
- Early recognition/seeking senior help
- Assess airway and breathing and administer oxygen if required
- Rapid vascular access
- Empiric antibiotic therapy
- Carefully titrated fluid resuscitation
- Early initiation of inotropes
- Early involvement of critical care services
- Source control
- Frequent reassessment
Approach to Management
Consider consultation with local paediatric team
Any child with suspected sepsis
Consider transfer to intensive care unit when
- Child requiring escalation of care beyond local centre
- Signs of shock persisting despite 40 mL/kg fluid
- Inotrope requirement
- Persistent venous serum lactate >3 mmol/L
- Neutropenia (<1000/mm3) unrelated to chemotherapy
- Large pleural effusion (near white out of the hemithorax)
- Coagulopathy (INR >1.6, APTT >60, Fib
<1)
Secondary resuscitation measures (second line inotrope/vasopressor, steroids, haemofiltration, ECMO) should be discussed with Retrieval Services or PICU
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services.
Parent information sheet
Sepsis (Health Direct)
Last Updated March 2020