See also
Code stroke pathway (RCH)
Anticoagulation therapy
Sickle cell disease
Endovascular clot retrieval pathway (RCH)
Neurology: Investigation and management of stroke (RCH)
Key points
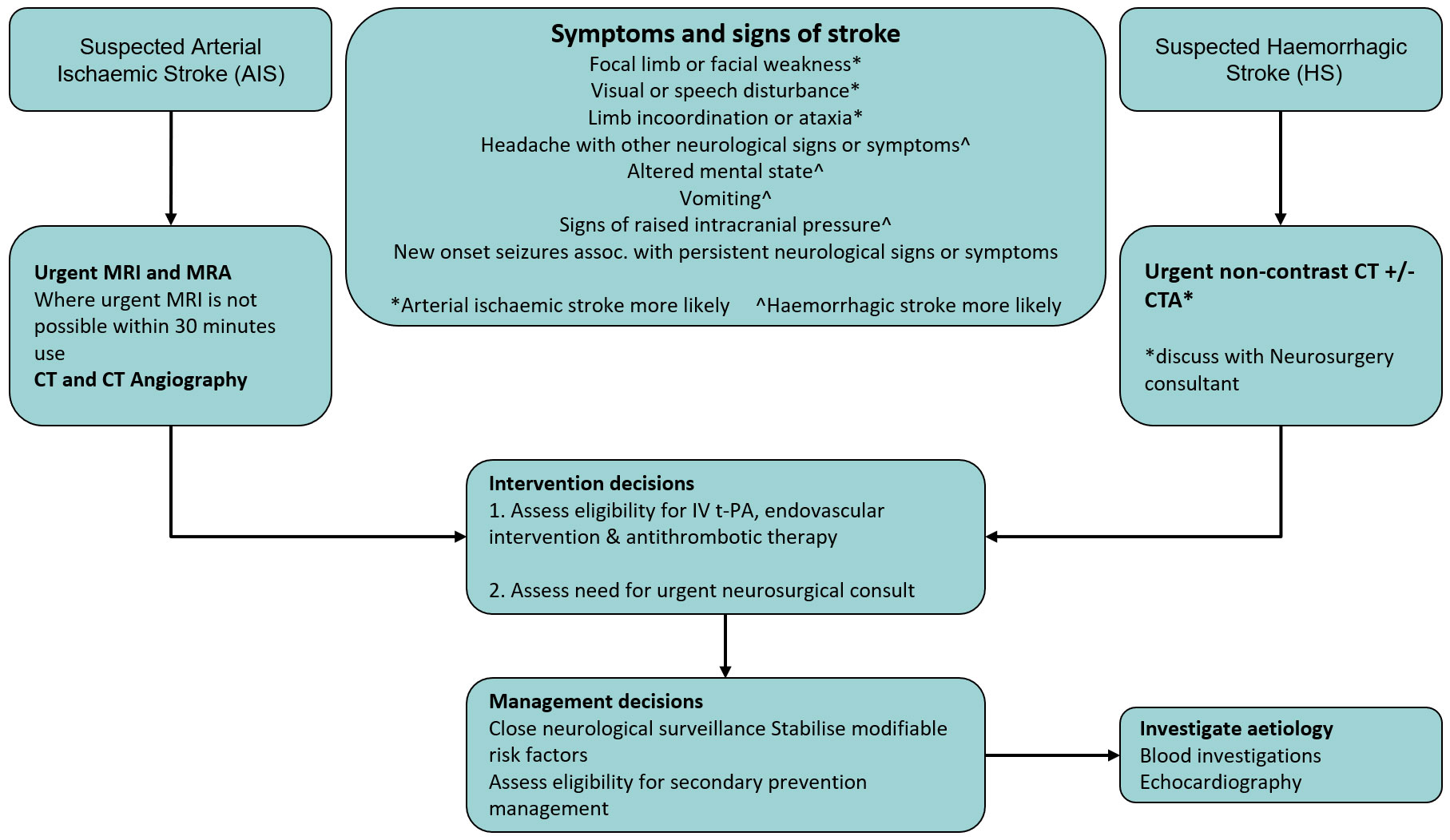
- Urgent
brain imaging is critical to confirm stroke diagnosis and guide management.
- Early involvement of a paediatric Neurology team is essential to guide assessment and acute management of suspected childhood stroke.
- Reperfusion therapies are time critical: alteplase within 4.5 hours, and endovascular clot retrieval within 6 hours of symptom onset.
Background
- Childhood stroke has a mortality rate of 5-10%. More than half of the survivors have long-term neurological impairment and 10-20% suffer recurrent strokes
- Arterial ischaemic stroke is the most common subtype, accounting for just over half of all strokes
Assessment
Red flag features
Children presenting with sudden onset of the following features are at high risk of stroke and should undergo immediate neurological assessment and be considered for urgent neuroimaging:
- Focal limb or facial weakness*
- Visual or speech disturbance*
- Limb incoordination or ataxia*
- Headache with other neurological signs or symptoms^
- Altered mental state^
- Signs of raised intracranial pressure^
- New onset seizures associated with persistent neurological signs or symptoms
*Arterial ishaemic stroke more likely ^Haemorrhagic stroke more likely
History
- Congenital heart disease
- Sickle cell disease
- Recent head/neck injury, chiropractic neck manipulation (risk factor for dissection)
- Methamphetamine or cocaine use
Examination
- Signs of raised ICP
- Hypertension
- Cardiac murmur
- Carotid or cranial bruit
Management
Investigations
Brain imaging
- In suspected haemorrhagic stroke, urgent non-contrast CT should be performed
- In suspected arterial ischaemic stroke, urgent brain MRI and MRA should be performed
- Where urgent MRI is not possible within 30 minutes, CT, including CT angiography should be performed
Immediate investigations to determine eligibility for reperfusion therapies
- FBE, coagulation profile, UEC, glucose, LFTs, blood group and hold
Subsequent investigations to identify underlying causes of confirmed stroke
- ECG and echocardiography
- Prothrombotic markers and serum homocysteine
Treatment
Initial stabilisation and maintenance of vital functions
In children with suspected or confirmed stroke:
- Oxygen if hypoxic
- If hypertensive, discuss with Neurology team before considering treatment
- Treat recurrent or prolonged symptomatic seizures. See
Afebrile seizures
- Avoid hyperthermia – aim to keep temperature ≤37.5oC
Reperfusion therapies
- Acute treatment decisions should be coordinated by the Neurology team in consultation with Emergency and Haematology teams
- Assessment of initial stroke symptom severity using the
Pediatric NIH Stroke Scale must be performed in consultation with the Neurology team before reperfusion therapy is commenced
Alteplase (recombinant tissue plasminogen activator) may be appropriate in specific children.
Potential eligibility criteria include:
- 2 to 17 years of age
- radiologically confirmed arterial stroke with absence of haemorrhage
- Pediatric NIH Stroke Scale score ≥4 and
<24, with symptoms that are not improving
- time from symptom onset
<4.5 hours
Administration: IV infusion - Total dose is 0.9 mg/kg (maximum 90 mg):
- bolus of 0.09 mg/kg
- then 0.81 mg/kg infused over 60 minutes
Absolute contraindications
- Known cerebral arterial venous malformation, aneurysm, or CNS neoplasm
- Known allergy to Alteplase
Endovascular therapies may be appropriate in some children with radiologically diagnosed ischaemic stroke (discuss with Neurology)
Anticoagulant and antithrombotic therapy
In children with arterial ischaemic stroke in whom reperfusion therapy is not given, or as secondary prevention:
- Anticoagulation and antiplatelet therapy are indicated after the exclusion of haemorrhage on brain imaging
- Anticoagulation and antiplatelet therapy should not be administered within 24 hours of receiving alteplase
Urgent neurosurgical consultation recommended for:
- Clinical signs of raised intracranial pressure
- Intracranial haemorrhage
- Malignant middle cerebral artery infarction
- Posterior circulation infarction
Consider consultation with local paediatric team when
All children with suspected stroke
Consider transfer when
All children with stroke should be admitted to a primary paediatric stroke centre
For emergency advice
and paediatric or neonatal ICU transfers, see Retrieval Services.
Last Updated July 2024