See also
Resuscitation: Care of the seriously unwell child
Recognition of the seriously unwell neonate and young infant
Cardiac telemetry
Key points
- Supraventricular tachycardia (SVT) is common in infancy and childhood. Most SVT in children is due to a re-entrant mechanism and usually occurs in otherwise normally well children
- Greater than a third of new onset SVT occurs in the first few weeks of life, commonly presenting after many hours with signs of heart failure
- Vagal manoeuvres should only be attempted in a child who is clinically stable
Background
- SVT is an abnormally fast heart rate originating from above the ventricles
- SVT is one cause of narrow complex tachycardia
- Younger children: usually caused by atrioventricular re-entry (AVRT), including Wolff-Parkinson White syndrome
- Adolescents: more commonly caused by atrioventricular nodal re-entry (AVNRT)
- Other causes: include sinus tachycardia, atrial flutter, ectopic atrial tachycardia and junctional ectopic tachycardia
- SVT typically has a fixed rate, usually >220 bpm. Onset and offset are abrupt, and p-waves are either not visible or seen after the QRS complexes (See additional notes below for important features when differentiating between different causes of narrow complex tachyarrhythmias)
- Always assume a broad complex tachycardia is due to VT rather than SVT with aberrancy, unless there is clear evidence it is not VT
- Factors that may contribute to tachycardia (eg sepsis, pain, dehydration, anxiety, and fever) should also be considered and addressed when managing a patient presenting with a tachyarrhythmia
Assessment
The priority is to identify the child in shock (pallor, poor perfusion, decreased consciousness, hypotension) and proceed immediately to resuscitation (see flowchart below)
|
|
Infants |
Children/Adolescents |
|
Feature |
Tolerate tachycardia well, making early signs and symptoms initially subtle |
Able to perceive palpitations and therefore present earlier with less clinical signs or symptoms |
|
History |
Parental concern for infant Irritability, poor feeding, lethargy and sweating |
Child complains of feeling ill, breathless, chest pain, nausea, dizziness or sweating |
|
Examination |
Typically present late, with signs of congestive heart failure (respiratory distress, hepatomegaly, oedema) |
Examination may be normal |
|
Red Flags
Unwell appearance, hypotension, drowsiness/altered conscious state
Note: BP machines and pulse oximeters may be unreliable at common SVT rates |
Management
Investigations
12 lead ECG (pre and post reversion techniques)
- Is there a tachyarrhythmia?
- Is there a broad or narrow QRS complex?
- Are P-waves present and what is their morphology?
- Is the rate fixed or variable?
(See additional notes below for further details)
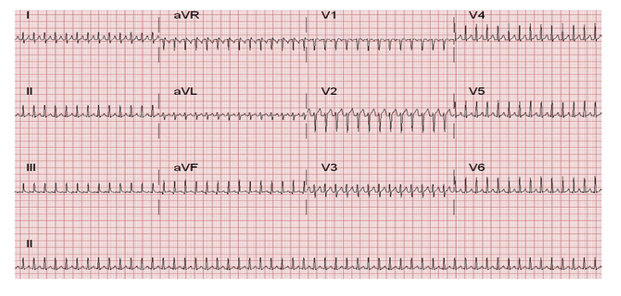
ECG Rhythm showing typical SVT
Other investigations
- CXR can be considered if clinical signs of heart failure present
- Blood tests provide no added benefit to the diagnosis or management and therefore are not recommended, unless considering other causes of SVT
Treatment
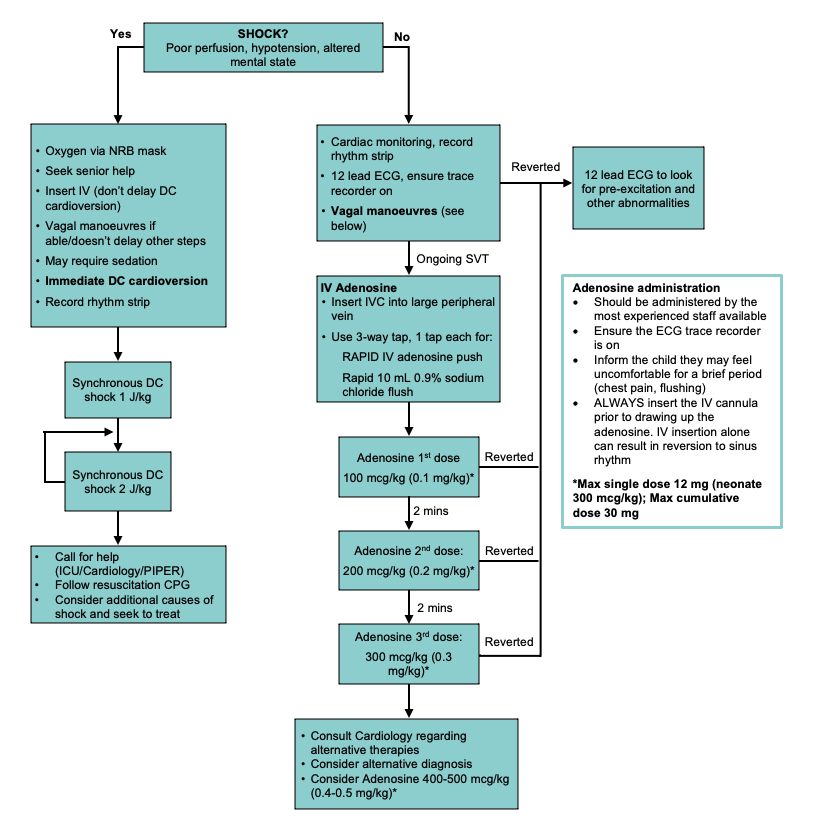
*Adapted from the Sydney Children’s Hospital Network Guideline on SVT
1. Vagal manœuvres
- Vagal manoeuvres are safe, minimally invasive and effective for reverting SVT in a hemodynamically stable child or infant
- Continuous cardiac monitoring should be applied prior to performing
- If unsuccessful, or child deteriorates, proceed to medical treatment as per the algorithm
DO NOT perform Eyeball pressure or carotid sinus massage as they are no longer recommended
Neonates and infants (<6 months)
- ‘Elicit the diving reflex’ with facial immersion in ice water for 5 seconds
- Facial immersion must not be used for infants in hemodynamic compromise/shock
- Carefully explain to the parents what you are doing and why
- The baby is attached to a cardiac monitor, arms are wrapped in a towel, and the whole face is immersed in an ice water slurry for five seconds. It is unnecessary to occlude the nostrils
- This technique is safe and 90% effective in terminating SVT
Older infants / Toddlers
- Apply an ice-cold facecloth or bag filled with ice slurry to the face for 15-30 seconds (elicits the ‘dive reflex’).
- While less effective than facial immersion, it is better tolerated in older infants
School-aged children
- Valsalva technique: with the child in the supine position, ask them to blow on their thumb or a 10 mL syringe, after full inspiration, for 10-15 seconds.
- There should be no air escape and the child should be seen to strain
- Modified Valsalva: manoeuvre performed as above in a semi-recumbent position. Then at the end of the strain, the child is immediately repositioned into a supine position with passive leg raise to 45 degrees.
- This has been demonstrated to significantly increase efficacy of the Valsalva manoeuvre (see
instructional video)
- Handstand is also a useful option with adult assistance if the child is well enough
2. Adenosine
- Adenosine has a very short half-life of 5-10 seconds. It acts by briefly blocking AV node conduction
- Always attempt to record a rhythm strip during adenosine administration as the response may be helpful in the diagnosis of the underlying tachycardia even if the tachycardia does not terminate (can use the defibrillator rhythm strip for this purpose)
- Adenosine side effects:
- Transient flushing and chest tightness/discomfort are relatively common side effects. These typically correlate to a brief pause on the ECG trace as the AV node is being blocked
- Rarely atrial fibrillation or prolonged pauses may occur
- Exacerbation of asthma due to bronchospasm (avoid in patients with history of severe asthma or active wheeze at time of experiencing SVT)
- Adenosine contraindications:
- Patients taking dipyridamole (Persantin) require a lower dose of adenosine
- For post cardiac transplant patients with a denervated heart, adenosine should be avoided if possible (risk of asystole or sustained bradycardia). If used, a lower dose is required. Consult cardiology
- Adenosine-deaminase deficiency (rare immune deficiency)
- Other Adenosine treatment considerations:
- Rapid re-initiation of tachycardia is not uncommon, mostly due to premature atrial contractions stimulated by the adenosine. If this occurs, discuss with Cardiology
- Beware of Adenosine changing re-entry SVT to atrial fibrillation, which can be dangerous if WPW is present. This will require DC cardioversion
- For children on theophylline, consult cardiology. Theophylline competes at the adenosine receptor and therefore children on this medication will require higher doses
3. Verapamil
- Contraindicated in children
<12 months, due to irreversible hypotension and lethal ventricular dysfunction
- Not routinely used in children, despite increasing use of calcium-channel blockade in adults for the management of SVT
Consider consultation with local paediatric team when
The child with the following often requires admission:
- first presentation
- under 3 months of age
- in heart failure
- requiring DC conversion
Children with known SVT having a breakthrough episode should be discussed with their usual Cardiology team where possible
Consider transfer when
Child is requiring care beyond the comfort level of the facility
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval Services
Consider discharge when
The child has reverted, not meeting the criteria for review/admission above, and observed for 90 min. Ensure follow up arranged
Additional Notes
|
Causes of tachyarrhythmias and differentiating clinical features |
|
|
Rate |
P-waves |
Variability |
Most common demographic |
|
Sinus Tachycardia |
<220 |
Present, normal morphology |
Variable |
Typically unwell children or systemic illness |
|
Supra Ventricular Tachycardia |
>220 (commonly 250-300 in infants) |
Absent or after QRS |
Fixed |
|
|
AVRT including WPW |
|
After QRS |
|
Neonates and children |
|
AVNRT |
|
Not usually visible |
|
Adolescent |
|
Atrial Flutter |
Up to 500 beats/min in neonates (300 beats/min in children) with variable AV conduction being common |
Saw tooth flutter waves (often only appreciated with AV block from adenosine) |
Fixed but may appear irregular depending on AV conduction |
Neonates (then not again until adulthood) |
|
Atrial Ectopic Tachycardia |
|
Precede QRS with abnormal axis |
Variable |
May not respond to DC cardioversion or adenosine. Can cause cardiomyopathy. |
|
Junctional Ectopic Tachycardia |
170-300 |
Inverted |
Variable |
Post cardiac surgery |
Additional Resources:
APLS algorithms
Acceptable Ranges for Physiological Variables
Emergency Drug and Fluid Calculator
Monash Hospital Paediatric Emergency Medication Book
Children’s Health Queensland Hospital and Health Service – Optimus Bonus: Supraventricular Tachycardia
Last updated January 2022