What is Continuous Glucose Monitoring (CGM)?
While blood glucose checking measures the Blood Glucose Level (BGL) via a drop of blood on a test strip, CGM works by a sensor measuring the glucose in the fluid around the cells under the skin (this is called interstitial fluid). The sensor is inserted under the skin. A transmitter connects to the sensor and sends the sensor glucose reading to a device (a phone, insulin pump or a Libre glucose meter). These are called Sensor Glucose (SG) readings
When glucose levels are stable and the system is correctly calibrated (if needed), the BGL and the SG are likely to show similar readings. When glucose levels are changing quickly (such as after giving insulin, eating, exercise or hypo treatment, or when you are unwell etc.) you should expect differences between the two readings. It takes time for the glucose to move from the blood stream into the interstital fluid area.
CGM systems currently available (for insulin injections)
Dexcom G6 CGM
Dexcom G7
From the 1st of March 2025 the Dexcom G7 CGM will be available via NDSS. There are a couple of things to be aware of if you want to upgrade to the Dexcom G7:
- It is not yet compatible with the Ypso insulin pump therefore Ypso users will need to continue to use the G6 until advised.
- The Tandem T-slim does provide compatibility with the Dexcom G7 and you can find more information here.
- Ensure you check your CGM menu for a G7 selection item on your Tandem t:slim pump. If you can't see this option, you need a pump upgrade (if out of warranty) or a software update (if in warranty), before changing to the Dexcom G7. AMSL will send out the information for a software update or please contact AMSL if you have not received these instructions. - Ensure the Dexcom G6 app or device is removed from you mobile phone and pump before starting G7.
- Log into the Dexcom G7 app using the same log in details as the Dexcom G6, there is no need to create new account.
- Check that your mobile phone is compatible with the G7 before upgrading.
To upgrade to the Dexcom G7, you will need to contact us at diabetes@rch.org.au or speak to us in diabetes clinic and request an update to your CGM information through NDSS. When you get email confirmation that this change has been processed, you will then be able to go to your chemist and collect your G7 as you would with your G6– we suggest that you advise your chemist to order in the G7 before you email us and check you have enough G6 supplies before requesting us to change to the G7 in case of any delays.
See instructions to using the Dexcom G7 and how to insert the Dexcom G7.
When using the G7 for the first time a key difference is the all in one insertion push the applicator down onto your skin and then push the button to insert your sensor, remove the applicator and then press down on the inserted transmitter for 10 seconds.
You can link to Clarity and the clinic's Clarity through the G7 app with the code 0393456661.
Libre 2 CGM
Medtronic Guardian 4 Smart CGM
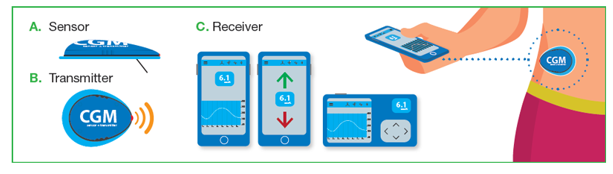
Image from NDSS website. Further information is availble from NDSS . Please click here
Dexcom Overpatch
Dexcom Sensor Overpatches for use with Dexcom G6 CGM sensors may help in keeping your sensor adhesive secure and clean. They are available at no charge if using a Dexcom sensor product - order here
Some limitations of CGM
It is important to understand that these systems are used in addition to, but do not completely replace BGL checking using finger pricks. Please read the “fine print” when companies write “no more finger pricks” or similar and privacy statement for access to technology
BGLs are checked:
To confirm the blood glucose when symptoms do not match the SG reading
When the sensor glucose is less than 4 mmol/L to confirm hypoglycaemia before treatment
After hypoglycaemia treatment to confirm blood glucose has risen above 4 mmol/L
When insulin is due and the sensor glucose reading is above 15 mmol/L
During “warm up” of the device. During warm up SG readings are not available
When the device disconnects or fails to give readings
To calibrate the sensor (if required by your chosen device)
When using CGM a receiving device is required. If parents want to follow and receive real time information, the receiving device will need access to wifi or have a data plan. NDSS funding for CGM is limited to the CGM, not the receiving devices or data plans.
Some benefits of CGM
- The trend graphs show glucose readings between blood glucose checks. Trend graphs can be used to interpret the effects on blood glucose of different foods and exercise. It also shows 24 hours of glucose trace, including overnight. Some parents find this reassuring
- CGM can be set to alert if the SG reading is above or below set glucose values
- Trend arrows indicate the rate of change in the SG reading. This can be particularly helpful during exercise or exams or while driving as it can prompt a blood glucose check. The glucose trend can also reassure parents when the glucose is in target and stable that extra carbohydrate is not required, reducing eating those extra carbs "just in case" a hypo occurs
- All companies have interactive reporting available showing insulin doses, carbohydrate eaten and exercise markers, however this information must be entered in by the user. The reports also show the trends in SG readings over different days, the time glucose has been within range and patterns in above or below target readings. This can be very helpful in reviewing insulin doses and carbohydrate intake.