Key goals of diabetes management
- prevent high glucose levels from occurring and
- to reduce the overall time spent with high levels.
This is because we know that exposure to hyperglycaemia (high glucose levels) increases the likelihood of developing health problems / complications related to diabetes over time.
Although your child may not feel differently when their level is above target, it’s important not to tolerate these levels as ‘being OK’
There will be times when glucose levels go above the target range and from time to time they may go very high.
Remember: if your glucose level is 15 mmol/L or higher, it is important to check your ketone levels. When ketones are 1.0 mmol/L or higher, they need immediate management.
Visit the Ketone advice page on how to manage ketones that are 1.0 mmol/L or higher.
This page aims to help you to learn how to work out how much insulin to give to help your glucose level come down back to the target range when you do not have elevated ketones.
If your continuous glucose monitor (CGM) is reading a glucose of 15 mmol/L or higher, it is important that you do a fingerprick blood glucose level (BGL).
A reminder on glucose targets
When looking at what we need to do to manage a higher glucose levels, it is important to remember what the target glucose levels are:
Target glucose levels
- 4–7 mmol/L pre meals
- Below 10 mmol/L 2–3 hours after eating
- Time in Range (4–10mmol/L) on CGM should be over 70% at a minimum and ideally above 75%
- Total time spent with high glucose levels above 10mmol/L should be less than 25% of any CGM period.
- Time spent with levels above 14mmol/L should be less than 5% of any CGM period (i.e. levels in this range should be rare)
If your child has a glucose level that is high, it is important to act to address this. On this page, we give you information on how to give extra insulin (‘a correction’) to treat a high level.
Note: if you are needing to do this frequently, then this means that your current insulin doses are not meeting your needs and they need to be changed.
If you see a pattern of glucose levels outside of target range across the day, a dose adjustment is needed!
Dose adjustment information to help with making changes to your overall insulin doses
What to do when your glucose is higher and your ketones are less than 1.0 mmol/L?
What to do if you do not know how much NovoRapid®/Humalog® insulin to give as a correction OR you need to re calculate how much to give as a correction?
If the glucose is high in between meals and ketones are under 1.0 mmol/L
Wait till the next meal, then add a correction of NovoRapid®/Humalog® at the next meal if the glucose is still high.
If the glucose is higher pre your main meal
A correction dose is required on top of the usual dose of insulin with food.
How to work out how much NovoRapid®/Humalog® insulin is needed to correct your glucose level (When you do not not have ketones)
Your child should be given advice about correction doses and correction factor in the weeks after diabetes diagnosis.
You may have a table as shown below but if you don't or it hasn't been reviewed for some time, this is how you work out how much extra insulin is needed to correct your glucose back to the target range:
There are a few ways to know how much insulin you need to help your glucose levels come down to the target range. The amount of insulin to give is based on what we call a correction factor (also called insulin sensitivity factor).
We describe it as: 1 unit of insulin will lower your glucose by ‘X’ number of mmol/L, where ‘X’ is the correction factor.
Step 1: Calculate your current total daily dose (TDD). To do this, add up all of your insulin doses for one typical day (long acting plus rapid acting)
Step 2: Calculate your correction factor = 120 ÷ your TDD
Step 3: Work out the correction dose (the amount of extra insulin needed to bring your glucose level back into range). This amount will vary, depending on your current glucose level and your correction factor.
- Go to this calculator to work out how much need to correct. If you do not have a carb ratio just keep this blank and fill in your Correction/ISF and Current BG and it will do the calculation for you.
- To do this calculation manually go through the following:
This is how you work out how much insulin you need at this time:
A. Calculate the correction gap to be treated: Current blood glucose level - Target glucose level (use 6 mmol/L) =
B. Calculate your insulin correction amount by dividing your correction amount (worked out in A) by your correction factor (Worked out in Step 2 above)
Correction amount ÷ correction factor = correction dose to be given
C. Add the ‘correction dose’ amount to your usual mealtime insulin dose (i.e. the dose that will cover food).
Example
If your current doses of insulin are:
Pre breakfast: 5 units NovoRapid®
Pre lunch: 6 units NovoRapid®
Pre dinner: 6 units NovoRapid®
Long acting: 12 units
TDD = 29 units (add up all of your NovoRapid® and long acting
e.g. glargine)
Let’s say, the current BGL is 18.4 mmol/L pre dinner. You check ketones and they are 0.3mmol/L. The dose of insulin to give before dinner can be calculated as follows:
Step 1: work out the correction factor 120 ÷ 29 (TDD) = 4 mmol/L
Step 2: the current BGL is 18.4 mmol/L - target (6 mmol/L) = Tells you the BGL needs to come down 12.4 mmol/L to come back into range
Step 3:
A. Work out the ‘correction gap’: the current BGL is 18.4 mmol/L - target (6 mmol/L) = 12.4. This tells you the BGL needs to come down 12.4 mmol/L to come back into range
B. Calculate the correction dose: 12.4 mmol/L (the amount the glucose needs to come down) ÷ 4 (correction factor) = 3.1 - round this to 3 units NovoRapid® as the dose needed for a correction on top of the usual meal time insulin.
C. In this example, the pre dinner dose is you have 6 units to cover food intake, so the pre-dinner dose to be given should be 6 + 3 = 9 units NovoRapid®
Important tips for correcting glucose levels
- Start with giving corrections before main meals/when rapid-acting insulin is being given anyway.
- In the first instance, start with giving corrections for all pre-meal glucose levels that are above 9-10 mmol/L, once you are confident in your correction factor, you can correct for pre-meal glucose levels above 7-8mmol/L.
- It’s important to assess the response to correction doses. The above calculations will give an estimate that is a good starting point but if your child’s glucose is not coming down to target range afterwards, the correction factor should be reviewed
and adjusted.
- Remember, when your child’s TDD changes, the correction factor will change too. It’s important to keep an eye on this and adjust it as per above.
- If your child’s levels 2-3 hours after corrections are still above 6mmol/L, the correction factor needs to be stronger.
-
If your child is having hypos after correction doses, this doesn’t mean you should stop giving them, you just need a different correction factor. Check their TDD hasn’t changed, or use 150 in the calculation in Step 2 instead. In the example
above, this would give a correction factor of ~5 and so the correction dose would be 2.5 units (12.4÷ 5 =2.5).
- If a correction is needed between meals, monitor the glucose levels closely after via CGM or by checking the BGL 2 hours after this additional dose has been given.
- Avoid correcting high levels immediately after exercise.
- Space NovoRapid
® doses 3 hours apart to allow insulin to not overlap
- If you are finding that when you do give a correction, the glucose stays higher or it comes down too much, resulting in a low glucose, the settings in the app or reader may need to be adjusted to reflect a change in the insulin dose. If you need support
with making changes contact the team diabetes@rch.org.au
Charts and apps to help with corrections
You can also use a correction chart or flexible bolusing to help you make the necessary adjustments:
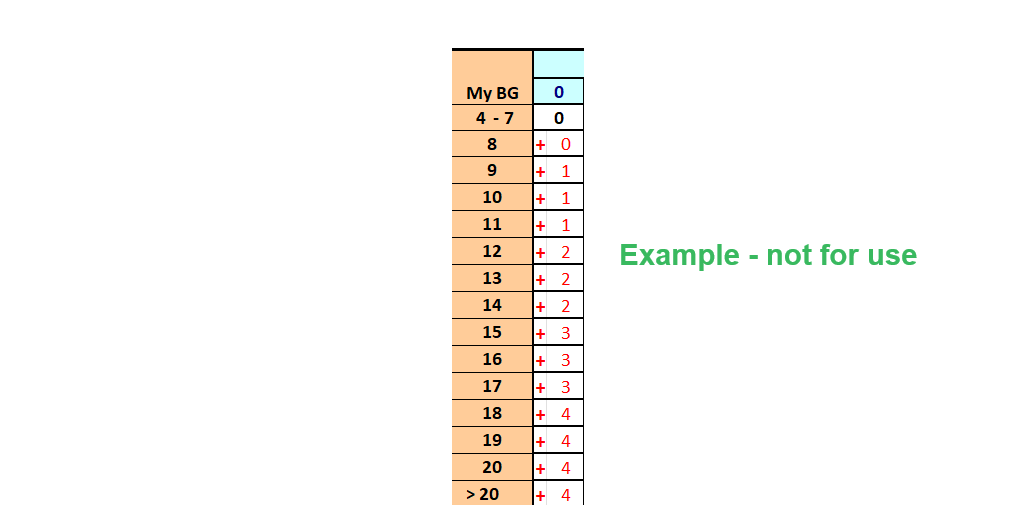
1. A correction chart, as shown below, shows the amount of extra NovoRapid®/Humalog® to be added to your usual dose before the meal. This is based on what your glucose level is currently reading.
- As your insulin doses change, the amount you need to correct a higher glucose level with changes as well, it is important to review this chart with your diabetes doctor in clinic.
- If you are finding that when you do give a correction, the glucose stays higher and doesn't correct enough or it comes down too much, resulting in a low glucose, the chart may need to be adjusted.
- You can email diabetes@rch.org.au to get support from the diabetes nurses to to keep this chart up to date.
2. Flexible bolusing is an ongoing way to include a correction in your meal time NovoRapid®/Humalog® insulin. See this page for more information and speak to your doctor in clinic about a referral for training.
Page last updated September 2024