Introduction
Gastrostomy tubes are inserted as an alternative or additional means of providing enteral feeds, fluids and/or medication for those who are unable to consume enough nourishment for their daily needs by mouth. Children may require a gastrostomy tube for
a variety of reasons including:
- Impaired oral feeding and swallowing
- Facial, oropharyngeal and or oesophageal structural abnormalities
- Anorexia related to a chronic illness
- Increased nutritional requirements
- Congenital anomalies
- Primary disease management.
Gastrostomy tubes can be used to:
- Administer bolus, intermittent or continuous feeds
- Administer Medication
- Facilitate free drainage and aspiration of the stomach contents
- Facilitate venting/decompression of the stomach.
Before accessing a gastrostomy, it is important to understand why it is in-situ, the type of device and when and how the device was inserted.
Aim
This guideline aims to support the care of patients with a gastrostomy tube in a safe and appropriate manner.
Definition of term
- Enteral feeding: a method of supplying nutrients directly into the gastrointestinal tract.
- Gastrostomy: The surgical formation of an opening through the abdominal wall into the stomach.
- Gastrostomy-Button: (Mic-Key™,
MiniOne®, Nutriport (Kangaroo™)) - skin level button gastrostomy tube inserted into a pre-formed stoma.
- Gastrostomy tube: inserted endoscopically or surgically through the abdominal wall and directly into the stomach.
- Long balloon gastrostomy tube:
(G-Tube or Mic G) – a gastrostomy tube that has a balloon on the inside and long extension on the outside. Often used in ED as a temporary tube and sometimes for longer term use in certain patient groups.
- Percutaneous endoscopic
gastrostomy tube (PEG): a gastrostomy tube which is inserted with the assistance of a gastroscope and held in place with an internal bumper and external fixator.
- GastroJejunal tube (GJ/PEGJ): A tube that is inserted into the gastrostomy stoma and extends into the jejunum. It has a port to access the stomach and a port to access the jejunum.
- Venting: Feeding tubes may be used to facilitate venting or decompression of the stomach from the accumulation of air during interventions such as High Flow Nasal Prongs, Non-Invasive or Invasive Ventilation.
Types of Gastrostomy Tubes





Images courtesy of Creative Studios RCH
Post Operative
Assessment
of a newly formed Gastrostomy
Feeding and medication administration
Note: The gastrostomy tube should not be used for the first 6 hours
post insertion. This includes administration of feeds, medications, and water, unless
otherwise indicated in the post- operative notes, or specifically ordered
by the insertion team.
- Refer to standard orders for post PEG insertions in EMR.
- Feeds are ordered by the medical team and/or dietitian, considering the nutritional needs and clinical condition of the child.
- Refer to the bookmarked note by the dietician with the specific grade up plan.
- Usually 6 hours NBM and nil
by gastrostomy post operatively, followed by continuous gastrolyte as per orders. If fluid is tolerated this will go to continuous feed, then grade up to bolus.
- If the patient is expected to be discharged over the weekend, the grade up note may also include the feed plan for home.
- Venting may commence any time, if required.
Seek medical review if
- feeds are not tolerated,
- pain is not well controlled,
- abnormal vital signs,
- irritability or parental
concerns,
- febrile within first 72
hours, or
- tube is accidentally removed.
For further information regarding feeding and medication administration via a gastrostomy please see RCH Nursing Guideline:Enteral Feeding and Medication
Administration Nursing Guideline
See RCH Nursing Guideline: Jejunal
Feeding for jejunal feeding.
Gastrostomy Position and Securement
- Assess the stoma and monitor the position of the tube as clinically indicated.
- Monitor for movement of the external disc which should sit flush with the abdomen.
- Surgical notes should reference where the external disc sits at skin level or at the top of the external disc. Tubes are marked at 1cm increments.
- Check for migration of the tube by checking markings on the tube daily (some tubes may not have markings, and these can be marked with a permanent marker).
- Consider tape above the disc to stop it from slipping.
- Inform the family of fixation placement and to monitor for changes.
- Secure the tube to minimise pulling. Options include vest/belt using Tubifast yellow for small and medium sized children or a catheter stabilisation device for children that are too large for Tubifast yellow (do not use compression bandages).
- Seek medical review if the
- measurement of the tube
differs from the notes,
- disc moves up the tubing,
- external disc appears too
tight, or
- There is excessive swelling.
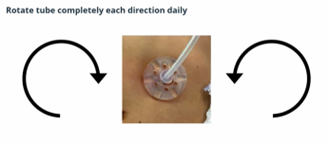
Tube rotation – Gastrostomy only
Rotating the gastrostomy tube helps to maintain a healthy stoma that is free of debris and helps prevent the inner bumper from becoming imbedded in the stomach lining (buried bumper)
NOTE:
Gastrojejunal tubes should NOT be rotated
- The gastrostomy tube should be
rotated (turned) starting 3-5 days after insertion. Confirm instructions with surgeon/gastroenterologist after insertion. Rotate the gastrostomy tube 360 degrees both clockwise and anti-clockwise daily. Seek medical advice if the tube does not rotate
easily.
- NOTE: For a surgically placed gastrostomy tube, the surgeon will advise the timing of the commencement of tube rotation. There may be a stitch in place to secure the disc from moving. In this case, consult with surgeon when to commence rotating
gastrostomy tube.
- The patient should be discharged with instructions on how to properly rotate the tube.
- Gastrostomy tube must be rotated, not just the disc. This ensures that the tubing that passes through the stoma, as well as the inner bolster is being turned.
![]()
Photo courtesy of RCH staff
NOTE: If the tube
does not rotate well, is very painful or bulging at the site of the stoma, the
patient requires URGENT medical review to assess for possible buried bumper.
Skin care
- Newly formed gastrostomies will sometimes have a split gauze topper insitu to manage post op ooze
- Follow any post op instructions regarding the dressing.
- If not contraindicated in post op note, change dressing when soiled.
- The stoma may require use of non-adhesive foam to absorbs ooze and assist in buffering movement. I.e. Allevyn™ or Biatain™.
Bathing
- Bathing/showering
may recommence 3-4 days after the initial gastrostomy insertion.
- Prior to this provide daily sponge baths avoiding the gastrostomy site.
- Clean the peristomal area with saline and gauze once or twice daily for the first 7-10 days.
Skin breakdown
- Try to determine the cause and administer treatment and prevent further breakdown
- Apply white soft paraffin as a skin barrier and a non-adhesive foam dressing to absorb and protect the site.
Seek medical review or refer to PEG clinic. Email PEG clinic peg.nurse@rch.org.au or call 55673 for review.
Ongoing Management of an established gastrostomy
Daily Care of established gastrostomy
Bathing and rotation of tube
- Clean around stoma and under external fixator once or twice daily. Use plain water or a soap-free wash (e.g. QV ™, Cetaphil ™). Pat dry, avoid rubbing to reduce risk of granulation.
- Rotate the gastrostomy tube 360 degrees both clockwise and anti-clockwise. If not bathing daily, tube rotation should still be done daily. Note do not rotate gastrojejunal tubes.
Dressings, and Skin Barriers
- Once oozing stops there is no need for a dressing, unless instructed by the PEG team or surgeon.
- If a dressing is required or preferred, use a non-Adhesive foam dressing, as it is absorbent and wicking.
- Example brands of non-adhesive foam dressings: I.e. Allevyn™ or Biatain™
- The dressing should be changed when wet through, or at least daily.
- A barrier can be used to protect the skin whilst there is ooze, or at any time when there is redness or leaking.
- Barriers to the skin include white soft paraffin (first line) and zinc creams, barrier wipes/wands/sprays.
Securement
- Monitor the fit of the gastrostomy tube when attending daily cleaning.
- Balloon volume does not need to be checked routinely; as this can contribute to premature balloon or valve failure.
- Balloon volumes can be checked if there is increased leakage from around the stoma or the tube appears looser than usual.
- Ask the parent/carer what the fit and leakage is typical like to avoid over-checking of the balloon.
- Use a firm singlet, all-in-one jumpsuit, tubular elasticised bandage or catheter securement device to prevent tubes from being accidentally pulled.
- Keep extension set disconnected when not using, if appropriate
- For children with feeds or access more often than every 2 hours, you may consider leaving the extension in place and securing it to prevent pulling. Regular connection and disconnection can contribute to stoma granulation formation and site
irritation.
- If
that patient has a balloon device, DONOT use the balloon inflation valve for food or medication administration. Feeds and medication should only be administered via the feeding port (see above diagram under types of gastrostomy tubes).
Other assessment considerations
- Regular weights (as clinically indicated).
- Referral to dietitian to review feeding plan.
- Referrals to speech therapy and/or occupational therapy.
- Bowel management (as clinically indicated).
Peristomal Leakage
Large amount of leakage (e.g. wetting clothing, soaking through dressing, visible food and milk from the stoma or visibly dripping from the stoma) needs medical review.
- Small volume of leakage is common and acceptable.
- Protect skin early, at first sign of leakage or erythema.
- See troubleshooting table for more information.
If large volume leak is not resolving, seek review.
Connecting Extension tubes
Mic-Key™
and MiniOne™
- Line up black line on extensions with black line on button.
- Push in firmly while holding both the button and the extension and turn clockwise maximum ¾ around.
- Care not to overtighten (relevant for ALL Enfit connections) as can lead to breakage.
- Twist to lock/unlock cap.
Kangaroo/Nutriport™
Twist all the way backward until the cap gives into the thread, then twist on Connecting extensions
- No lining up required
- Push in extension firmly using a flat finger on the top, while anchoring the button underneath (always 2-handed)
- If giving a long/continuous feed, use the yellow clip to secure the extension to prevent accidental disconnection. The flat side goes on the top of the extension and the 2 little tabs go under the button
Disconnecting
- Hold center of button firmly, grasp extensions from hard plastic connector (not from rubber tubing as this will break) and pull straight out
Note: Kangaroo™ buttons are no longer being used, but may still be in circulation until 2027
Note: that the extensions between Mic-key™, MiniOne® and Nurtiport™ (Kangaroo) are NOT interchangeable and therefore the correct extension needs to be sourced.
Troubleshooting gastrostomy tubes
|
Potential
problems
|
Cause
|
Action
|
|
Accidental
removal of initial PEG/G-tube
|
- Inner retention disk or balloon may have perished or deflated.
- Tube has been pulled out with force.
|
- Cover the stoma to prevent mess.
- Immediately contact the primary insertion team (i.e. Gastroenterology or Surgical team).
- Do not put anything in the stoma unless advised by the insertion team.
- Keep the patient NBM until receiving further advice from the insertion team.
|
|
Balloon tube
falls out (established PEG)
|
- Deflated or ruptured balloon or pulled out inflated.
|
- Wash with water and soap and reinsert the old tube (even if the balloon is ruptured) and tape to secure to keep the stoma patent while awaiting a fresh device.
Refer to RCH Clinical Practice Guideline: Gastrostomy acute replacement of
displaced tubes
|
|
Leakage from around gastrostomy tube
|
Tube too small for opening.
|
- Apply paraffin to skin generously and a foam dressing changed as wet, or at least daily.
- Consider adding stomahesive powder to stoma opening if site remains very wet.
- Seek medical review if leaking not manageable.
|
|
Tube migration into stomach. (Initial PEG)
|
- Adjust skin retention disc to ensure internal flange or balloon is snug against the inner stomach wall.
|
- Patient is unwell,
- More acidic gastric secretions and slower gastric emptying.
|
- Protect the skin while unwell. Reassure that it will likely improve when well again.
- Apply generous and frequent barrier ointment such as paraffin to minimise irritation to skin.
- Use absorbent foam dressings and change when wet.
- Consider stomahesive powder to stoma opening if leaking still persistent.
- Leakage should decrease as the child becomes well. If not, family to book PEG clinic appointment on discharge
|
- Patient has a GJ tube
- Jejunal extension has migrated into the stomach
- The tube has split above the jejunum
|
- Cease feeds if patient is unsafe for gastric feeds
- Advise the admission team
- Arrangement for assessment and possible replacement of the tube needs to be made with Medical Imaging by the treating team
|
|
Irritation,
skin redness, bleeding, soreness, swelling and oozing
|
- Tube leakage.
- Child is currently unwell with intercurrent illness.
- Skin infection
|
- Check balloon volume is optimised:
- Check balloon with a 10 mL luer slip syringe from the size port. Withdraw all of the water while holding the device in place.
- Have a second syringe ready with the correct balloon volume ready to reinsert.
- See Gastrostomy learning package (Learning Hero) for volumes.
- Apply a barrier cream to protect skin from moisture and acid.
- Apply a foam dressing to absorb and wick away leakage and exudate. Avoid use soft-wick gauze that will not wick.
- Hydrocolloid powder can help stop bleeding and absorb excess moisture.
- Seek medical review and consider acid reducing medications and need for swab or antibiotics or antifungal cream.
|
| Leakage through the low-profile tubes |
- Internal valve is not functioning well enough.
- Possible constipation or slow gastric emptying.
- Port may be plugged with medication, food Broken tip/locking notch from extension or valve may have stiffened and worn out.
|
- Manage constipation.
- Slow feeds.
- Flush the tube with a pulsatile action to assist in removing anything caught in the valve.
- If not resolving, either keep the tab/cap closed or extension plugged in at all times.
|
| Blocked tubes |
- Poorly crushed medications.
- Not flushing the gastrostomy tube when feeds are completed.
- The feed is too thick.
- Leaving formula in the tube to curdle.
- Blended food being put down the tube that are not blended thoroughly
- Feed contains lumps of powder.
|
- Flush with 10 – 20mLs of warm water using a gentle push-pull motion.
- Repeat a few times and if fails, the tube may require replacing.
- Do not use excessive force, Coca-ColaTM or other carbonated drinks.
See RCH Nursing Guideline: enteral feeding and medication administration guideline for more information |
| Granulation Tissue |
Rubbing, bumping, pulling, tube too tight or too loose. |
Remove/reduce cause of friction
- Secure heavy connectors to minimise movement and pulling.
- Initial PEG or long balloon tubes - check the disc isn’t too tight causing pressure and rubbing or too loose causing tube to be very mobile.
- Button devices – check device isn’t sitting too loose or too tight. Adjust balloon volume, using a 10ml Luer tip syringe and water. See Gastrostomy learning package (Learning Hero) for volumes.
- Protect site with foam dressing.
Absorb exudate and apply pressure
- Apply foam dressing (e.g. Allevyn™, Biatain™)
- Use in conjunction with other treatments for granulation.
- Refer to video ‘making and placing foam for a PEG/Button’ in the Gastrostomy Learning Package on Learning Hero.
Discuss further treatment with medical team and consider:
Reduce microbial load
Reduce inflammation – topical steroid
- Steroid cream ceased when resolved.
- Repeated, long term use of steroid cream causes the peristomal area to atrophy and can make long term gastrostomy sites difficult to manage.
- If the site quickly becomes irritated after ceasing steroid, then consider a barrier such as soft Paraffin and foam dressings instead.
|
| Broken Adapters on initial PEG |
- Inappropriate opening and closing techniques
- Not cleaning
- Connecting to lines and syringes too tightly
- Use of certain oils such as MCT and CBD
|
- Replacements sourced through PEG clinic or Nutrition department
- Advise parents how to open/close correctly.
- Recommended that rural/regional patients have a spare adapter available to take home and are shown how to change them.
- Those using oils that degrade the tubes quickly will need to purchase and keep extra adaptors.
- Vigilant flushing and cleaning of the adaptors may also assist in prolonging their life
|
| Broken or missing low profile extension tube |
- Connecting to lines and syringes too tightly
|
- Tubes can be sourced through EDC/dietician during business hours. If the patient does not have their extension or it is broken/ lost, wards can purchase the tubes from EDC. Outside of business hours, there is access to a small emergency
supply inside the PEG clinic, level 2, Day Med Unit or contact afterhours nurse coordinator.
|
| Buried Bumper |
- Inner bumper has migrated into the tissue between the stomach and the outside of the abdomen.
- Can occur due to poor healing, an outer disc that is too tight or a tube that is not well secured and gets pulled
|
- If the tube does not rotate well, is very painful or bulging at the site of the stoma, needs URGENT medical review.
|
Discharge home with a gastrostomy
Considerations
- Referral to Wallaby or Post Acute Care, if required
- Where possible, the child should be empowered by staff and family to contribute to the management of their gastrostomy.
- PEG clinic referral for 2–4 week review booked pre discharge.
- Ensure the family have the PEG Basic Care Guide available on the Gastroenterology PEG clinic and Gastrostomy Care site.
- Use the smart phrase .PEGEDU to guide and keep education and documentation.
- Ensure the family knows how to book a PEG clinic appointment-outpatient contact center 9345 6180.
- Dressings and securement devices can be purchased from EDC during business hours.
Links
Evidence Table
| Reference
|
Source of Evidence
|
Key
findings and considerations |
| Friginal-Ruiz, A. B. RN; Lucendo, A. PhD, MD, FEBGH. (2015). A Practical Overview on Its Indications, Placement Conditions, Management, and Nursing Care. Gastroenterology Nursing 38(5): p 354-366. DOI: 10.1097/SGA.0000000000000150 |
Literature overview
|
- Nursing care of patient with PEG
|
Pars, H. PhD, RN; Cavusoglu, H. PhD, RN. (2019). A Literature Review of Percutaneous Endoscopic Gastrostomy Dealing With Complication. Gastroenterology Nursing 42(2): p 351-359. DOI: 10.1097/SGA.0000000000000320
|
Literature review
|
- Risk factors for granulation tissue
- Causes of leakage
- Infectious complications
|
| Roveron, G.; Antonini, M.; Barbierato, M.; Calandrino, V.; Chiurazzi, L.; Coniglio, G.; Gentini, G.; Marchetii, M.; Minucci, A.; Nembrini, L.; Neri, V.; Trovato, P.; Ferrara, F. (2018). Clinical Practice Guidelines for the Nursing
Management of Percutaneous Endoscopic Gastrostomy and Jejunostromy (PEG/PEJ) in Adult Patients. Journal of Wound, Ostomy, and Continence Nursing 45(4): p 326-334. DOI: 10.1097/WON.0000000000000442 |
Executive summary of guidelines
|
- Post op management of stoma and tube
- Nursing management of common complications
|
Royal Children’s Hospital. Gastrostomy- Common problems.
https://www.rch.org.au/clinicalguide/guideline_index/Gastrostomy_Common_problems/
|
Clinical practice guideline |
- Management of blocked tube
- Leakage
- Excoriation and infection of skin
|
| Sick Kids. (2019). G/GJ tubes: Hypergranulation tissue. https://www.aboutkidshealth.ca/ggj-tubes-hypergranulation-tissue |
Clinical guideline |
- Signs, causes, and treatment of hypergranulation tissue
|
| Southeaster Sydney Local Health District. (2021). Wound - Management of Hypergranulation Tissue. https://www.seslhd.health.nsw.gov.au/sites/default/files/documents/SESLHDPR%20400%20-%20Wound%20Management%20of%20Hypergranulation%20Tissue_0.pdf |
Policy and procedure
|
- Management of hypergranulating tissue
- Removing or treating cause of friction to tissue
|
Starship Hospital. (2024). Gastrostomy.
https://starship.org.nz/guidelines/gastrostomy/
|
Clinical guideline |
- Initial and long- term management of gastrostomies
|
Please remember to
read the disclaimer.
The development of this nursing guideline was coordinated by Carla Rogers, CNC,
Gastroenterology & Clinical Nutrition, approved by the Nursing Clinical Effectiveness Committee. First published August 2024.