Introduction
Temperature management is a significant component of the care required for all neonatal and paediatric patients. Infants and children are susceptible to temperature variations due to physiological and anatomical differences. This includes their larger
surface area to volume ratio and immature thermoregulatory mechanisms. Monitoring and rapid intervention are critical. Careful consideration should be given to neonates undergoing general anaesthesia, it is recognised that perioperative hypothermia
at times may be unavoidable, however steps to mitigate risks should be undertaken. Body temperatures outside normal ranges may be indicative of underlying disease processes or clinical deterioration and should be identified within a timely manner.
Maintaining a stable body temperature within normal ranges assists in optimising metabolic processes and bodily functions. Therefore, minimising environmental factors within the hospital setting which may result in unnecessary body temperature fluctuations
is important.
Aim
To assist clinicians working at The Royal Children’s Hospital undertake the appropriate assessment and management of neonatal and paediatric temperatures.
Definition of Terms
- Cold stress is a cascade of physiological events caused by the infant’s use of chemically mediated thermogenesis in attempt to increase core temperature. Two specific alterations to thermogenesis occur in the infant suffering cold stress; vasoconstriction
of the peripheries, which allows heat to be drawn back to the core and metabolism of brown adipose tissue
- Heat
stroke: A presentation of severe hyperthermia. Thermoregulation is overwhelmed by excessive metabolic production and environmental heat, in combination with impaired heat loss. This is uncommon within an inpatient setting.
- Hyperthermia: An elevated body temperature due to failed thermoregulation. This occurs when the body produces and/or absorbs more heat than it can dissipate.
- Hypothermia: An abnormally low body temperature, where the body temperature drops below a safe level. Both low temperatures and hypothermia can be caused by environmental factors, metabolic complications, disease processes, or can be medically
induced.
- Normothermia: Body temperature within normal values.
Exact normal temperature ranges differ between individuals and can be influenced by some genetic and chronic medical conditions. It is important to ascertain the baseline for individual
patients in order to identify abnormal body temperature deviations. - Pyrexia: An elevated body temperature due to an increase in the body temperature’s set point. This is usually caused by infection or inflammation. Pyrexia is also known as fever or febrile response.
Some causes of fevers do not require medical treatment, whilst other causes need to be identified and treated. - Skin to skin
care (also known as kangaroo care): is the practice of holding an infant in an upright position, skin-to skin, on the parent’s chest for a period of time. Infant need to be stripped down to the nappy and nothing between them and their parent.
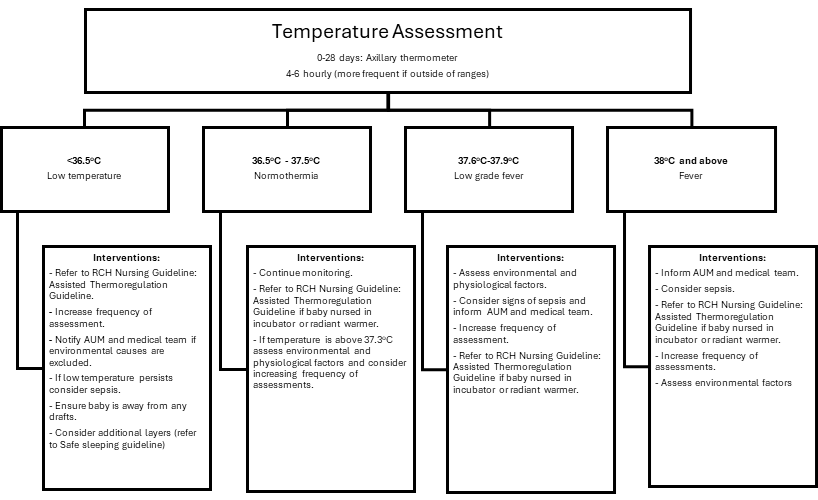
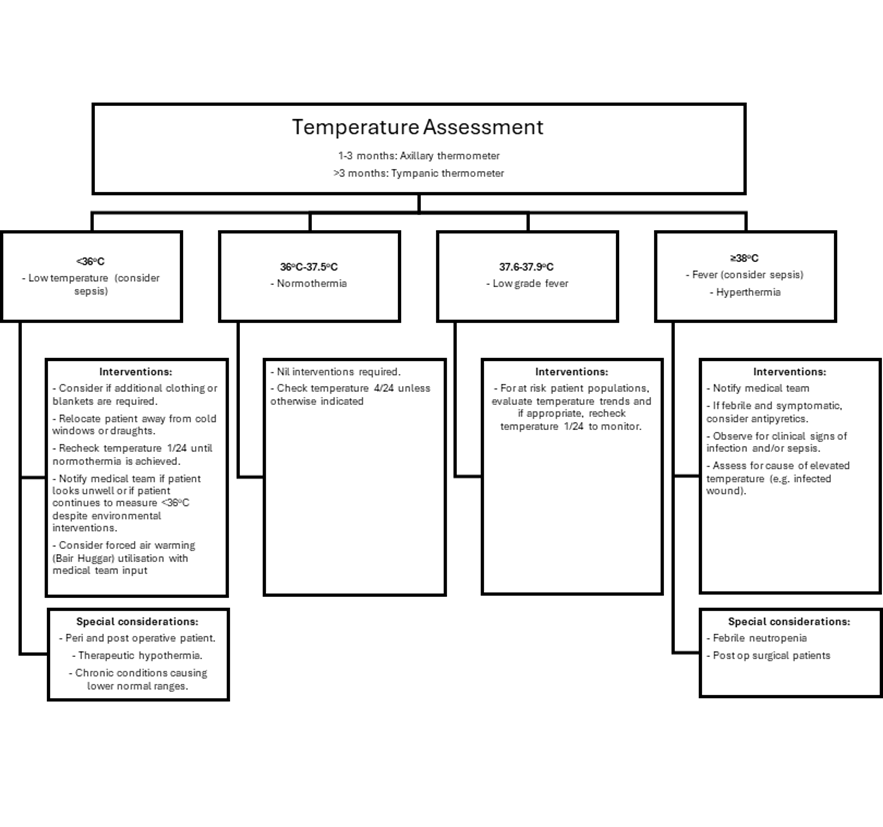
Temperature Ranges*
|
Classification
|
Neonates
|
Paediatrics*
|
|
Low temperature (or hypothermia)
|
<36.5⁰C |
<36⁰C |
|
Normothermia
|
36.5 - 37.5⁰C
|
36 - 37.5⁰C
|
|
Low grade fever
|
37.6 - 37.9⁰C
|
37.6 - 37.9⁰C
|
|
Fever (or
hyperthermia)
|
≥ 38⁰C
|
≥ 38⁰C
|
*Significant variation of suggested temperature values and ranges exists within current literature. The values presented in this table are derived from a collaboration of multiple sources and expert opinions and should be utilised as a guideline only.
It is important to ascertain an individual’s baseline in order to identify the possible cause/s of the temperature taken.
Please note, any febrile child who appears seriously unwell should have a
thorough assessment and their treating medical team notified, irrespective of
the degree of fever.
In infants less than3 months,
hypothermia or temperature instability can be signs of serious illness.
Assessment
- Body temperature should be measured on admission and four hourly with other vital signs, unless clinically indicated for more frequent measurements.
- Body temperatures falling outside normal ranges should be monitored and further managed where appropriate until normothermia is achieved.
- When assessing body temperatures, it is important to consider patient-based and environmental-based factors, including prior administration of antipyretics and recent environmental exposures.
- Body temperature should always be evaluated in the context of other vital signs and overall patient presentation.
Methods of body temperature measurements
Due to temperature variation between body sites, ideally the same route should be used for ongoing patient observations, as to allow for accurate temperature trend evaluation. Document the route used in EMR.
0-3 months: Axillary Route
Axillary digital thermometer is the preferred method for this age group, in most cases. This is the most accurate temperature measurement in neonates used for all patients on Butterfly.
Procedure
Place thermometer tip in the centre of the armpit over the axillary artery, ensuring skin is dry and intact prior to probe placement.
- Place the patient’s arm securely against their body.
- Turn thermometer on. For a more accurate reading, wait >3 minutes with thermometer in situ before obtaining a measurement.
0-3 months: Rectal Route (if
requested)
In some circumstances, a rectal temperature may be required for a more accurate assessment of body temperature.
This should be performed only if approved by medical staff, with ANUM involvement.
Rectal measurements should be avoided within the oncology population and in patients with low platelets, coagulopathy, or perineal trauma and pelvic area surgery, due to the increased risk of bowel perforation.
Procedure:
- Place plastic sheath over thermometer.
- Dab a small amount of lubricant on end of thermometer.
- Carefully insert thermometer 2cm into the infant’s anus (1cm for pre-term infant). Over-insertion may cause bowel perforation.
- Turn thermometer on.
- Wait for 5 seconds post Celsius sign flashing before taking a recording.
- Remove and clean thermometer with alcohol.
Over 3 months: Tympanic Route
Tympanic thermometer is the preferred method for this age group.
Procedure:
- Gently insert probe into ear canal until the canal is entirely sealed off, ensuring the tip is facing the eardrum.
- Press the thermometer button and wait for the beeps.
- If ears have been covered (e.g. headphones/beanie), remove items and wait until ear canal is cooled before taking measurement. If a patient’s ear canals are too small to properly insert the tympanic probe, consider an axillary thermometer route instead.
Notes:
If the patient has been exposed to cold environmental conditions, allow for adequate time for patient to stabilise within room temperature before measuring body temperature. For example, temperature will be lower if taken immediately following a bath/shower
or a procedure/dressing that requires a large body surface area to be exposed.
Both axillary and tympanic routes measure temperatures lower than true core body temperature.
Temperature measurement frequency may differ in sub-speciality areas, such as within the Emergency Department, critical care and peri-operative areas.
Please refer to specific department guidelines for further information.
At Risk Patient Groups
The following patient populations are at an increased risk of being unable to maintain normothermia:
- Neonates and young infants
- Peri and post-operative patients
- Neurologically compromised patients
Management
Preventative Approaches
A patient’s surrounding environment can greatly impact their ability to maintain an otherwise stable body temperature. Acknowledging and minimising environmental influences on thermoregulation is important for all paediatric patients, especially the neonatal
and at-risk patient populations.
The table below outlines approaches nurses, clinicians and families can utilise towards minimising preventable heat transfer from patients to their surroundings.
|
Mode
|
Definition
|
Clinical
Scenario
|
Preventative
Management
|
|
Evaporation
|
Heat loss occurring during conversion of liquid to vapour
|
Sweat, incontinence
Wet or oozing dressings
|
Keep patient dry
Remove wet clothing, replace wet dressings if appropriate
|
|
Convection
|
Transfer of heat from the body surface to the surrounding air via air current
|
Air drafts in room
|
Relocate patient away from draughts, close door
|
|
Conduction
|
Transfer of heat from one solid object to another solid object in direct contact
|
Cold blankets, cold weighing scales
|
Cover cold surfaces with pre-warmed towel or blanket
|
|
Radiation
|
Transfer of heat to cooler solid objects not in direct contact with the body
|
Nearby cold windows or walls
|
Relocate patient away from cold surfaces
Close blinds on window
|
Neonatal Considerations
Special Considerations for Neonates
Hypothermia
Neonates in the hospital setting frequently require a large portion of their body surface area exposed for assessment and procedures. This, combined with prematurity and illness places them at an increased risk of hypothermia. Hypothermia can progress
to cold stress, the neonate can develop increase oxygen requirements, respiratory distress, bradycardia, hypoglycaemia and acidosis. Therefore, it is imperative to optimise temperature regulation.
- Skin to skin care is a useful intervention to improve thermoregulation and should be encouraged when possible.
- Initiate forced air warming early if indicated and closely monitor. Stepped approach to rewarming is recommended. Aim to raise temperature by 0.5-1 degree per hour. For further information on forced air warming please refer to the Perioperative
section of this document.
- Contact Butterfly team for support and guidance for neonates outside the department.
- If transferring neonates for imaging or to the perioperative department, please ensure that patient is appropriately warmed using the radiant heaters to mitigate the risk of inadvertent hypothermia. Ensure they have warm blankets and beanie.
For further information on the management of neonatal patients and equipment required to assist with
thermoregulation such as radiant warmers and incubators please see the RCH
Nursing Guideline: Thermoregulation_for_neonates_and_infants
Paediatric Management
Notes:
- Sepsis: Early recognition and initial management of sepsis in neonates and paediatrics is paramount, and if left untreated can lead to severe morbidities and mortality. For further information on sepsis recognition and management of neonates and
paediatrics, please see RCH
Clinical Practice Guideline: Sepsis assessment and management
- Bair
Hugger devices: If using a forced air warming device outside of the critical care environments OT, PACU, PICU, NICU and ED, the temperature of the device should not be set to greater than 32⁰C in the inpatient setting. The patient’s temperature
should be rechecked at a minimum of every 30 minutes or if the patient is less than 6 months, a minimum of every 10 minutes whilst forced air warming in use, as patients are at a risk of overheating. Check that the blanket is connected to the
device correctly as patients are at risk of burns.
Special Considerations
The following patient populations may require more specific interventions and/or differing management when body temperature falls outside traditionally normal values:
Some patient populations have conditions that affect their basal metabolic rates and thus, have unique normal temperature ranges. It is important to ascertain these individual’s normal temperature fluctuations to identify abnormal readings and manage
appropriately.
Perioperative and Post Operative Patients
Preoperatively
- Ensure temperature is taken on admission and patients are appropriately dressed and consider active warming if indicated preoperatively.
- Provide a warm blanket if patient’s temperature is between 35.5⁰C and 36⁰C.
- Initiate forced air warming for patients less than 35.5⁰C if clinically indicated. Escalate to treating anaesthetist
- For neonates
- Continue the neonates current thermoregulation i.e., radiant warmer and consider use of warm blankets as needed
- Initiate forced air warming for neonates if patient temperature is
< 36.5
- In consultation with the anaesthesia team, consider preoperative forced air warming blanket for all patients if indicated and tolerated by the patient.
Anaesthesia
Consider forced air warming for all patients undergoing anesthesia and surgery, especially:
- Neonates
- Cases greater than 30 minutes with large areas of exposed skin
- History of CP/Musculoskeletal disorder where thermoregulation is impaired
- Patients undergoing major surgery such as orthopaedic procedures, laparotomies and large tumour removal with open body cavities.
- Patients with burns
Intraoperatively
- Active warming
via forced air warming (Bair Hugger / Cocoon) is recommended for patients
undergoing surgery when clinically indicated
- All patients with major burns where forced air warming devices are unable to be used should be placed on a heating mat (that is activated by the pressure of the patient lying on it).
- Patients with major burns, neonates and patients undergoing free flap surgery should have the ambient temperature in theatre increased in consultation with the anaesthesia and surgical teams.
- Theatre warming cabinets set to 40⁰C where irrigation fluids, IV fluids and blankets can be sourced from.
- Use warm irrigation fluids were possible.
- Apply warm blankets if patient is exposed or being transferred.
- Neonates: ensure that radiant heaters are used, preheated prior to patient transfer from theatre. Neonates should be kept warmed with beanies, blankets and appropriate clothing.
Recovery
- Ensure temperature is taken on admission to PACU and 15 minutely thereafter
- Initiate active warming via forced air warming (Bair Hugger/Cocoon) if neonatal patient temperature is less than 36.5⁰C or paediatric patients' temperature whose temperature is less than 35.5⁰C.
- Temperature should be taken every 5 minutes whilst a patient is receiving active warming.
- If overheating or burns occur, stop active warming and seek anaesthetic review (treating or in charge). Cool patient if appropriate. Document event via EMR and complete VHIMS.
- Patients with chronic conditions which cause lower baseline body temperatures should return to their baseline prior to transfer to ward. This baseline temperature should be discussed with parents/caregivers and communicated to the receiving ward or
day surgery.
- Discharge temperature is greater than or equal to 36.6⁰C for neonatal patients and greater than or equal to 36⁰C for paediatric patients. Ensure clinical indicators are completed and active warming interventions are documented in EMR.
- If the post-operative temperature is less than 36⁰C but greater than or equal to 35.5⁰C, for paediatric patients and the patient is rousable and all other vital signs are stable and within normal range, they can be transferred to in-patient units.
If clinically indicated, forced air warming can be made available to the in-patient units for continued use. This should be discussed with parents/caregivers and communicated to admitting unit.
Family Centred Care
Encourage parents and caregivers, where appropriate to provide skin to skin care for their infants. See RCH Nursing Guideline Skin to Skin Care for the newborn.
Educate parents and caregivers on recognising temperature changes of their child and escalate concerns to nurse or clinician caring for their child.
In the Perioperative setting, ensure that parents and caregivers are informed of the benefits of keeping their child appropriately warmed prior to anaesthesia & surgery.
Companion Documents
- RCH Nursing Guidelines
- RCH Clinical Practice Guidelines
- RCH Policy & Procedures
- ViCTOR Charts
Additional Useful Links
Evidence Table
| Reference
|
Source of Evidence
|
Key findings and considerations |
Bharti, P., Chauhan, M., & Ahmed, K. (2017). Comparison of rectal, infra-red tympanic and infra-red skin temperature in term neonates. International Archives of Integrated Medicine, 4(3), 43-49.
|
Single site retrospective study.
|
- Indications of measurement of temperature in paediatrics.
|
Burke, Dawn PhD, CRNP, NNP-BC; Lou Short, Billie MD. Perioperative Hypothermia in NICU Infants: Its Occurrence and Impact on Infant Outcomes. Advances in Neonatal Care 14(3):p 154-164, June 2014.
|
Evidence from single site study
|
- Findings have lead to nursing practice guidelines on neonatal thermoregulation to be reviewed. Recommendations include the use of hats to maintain temperature, prewarming of incubators and use of bair hugger for all neonates regardless of length of procedure.
|
Brozanski BS, Piazza AJ, Chuo J, et al. STEPP IN: Working Together to Keep Infants Warm in the Perioperative Period. Pediatrics. 2020;145(4):e20191121
|
Evidence from literature review
|
- Strategies to maintain perioperative euthermia in infants, including prewarming the OR and compliance with maintaining euthermia at key time points, can reduce postoperative hypothermia.
|
Considine J, Brennan D. Emergency nurses’ opinions regarding paediatric fever: The effect of an evidence-based education program. Austral Emerg Nurs J 2006; 9:101-11.q
|
Evidence from a quality improvement project.
|
|
Cronin JA, Soghier L, Ryan K, Shen C, Bhattarai S, Rana S, Shah R, Heitmiller E. A Quality Initiative for Reducing Postoperative Hypothermia for Neonatal Intensive Care Unit Surgical Patients. Pediatr Qual Saf. 2020 Jul 7;5(4):e318.
|
Evidence from a quality improvement project |
- Implementation of a quality improvement project which included the use of a perioperative checklist. The incidence of hypothermia following surgery decreased from 9.7% to 2.5% and this changed was sustained for greater than 12 months.
|
El-Radhi A.S. (2018). Measurement of body temperature. In El-Radhi A. (Ed.) Clinical Manual of Fever in Children (pp. 69-84). Retrieved from https://doi.org/10.1007/978-3-319-92336-9_4
|
Evidence from a clinical manual.
|
- Indications of measurement of temperature in paediatrics.
|
Elaine L. Duryea, David B. Nelson, Myra H. Wyckoff, Erica N. Grant, Weike Tao, Neeti Sadana, Lina F. Chalak, Donald D. McIntire, Kenneth J. Leveno, The impact of ambient operating room temperature on neonatal and maternal hypothermia and associated morbidities: a randomized controlled trial, American Journal of Obstetrics and Gynecology,Volume 214, Issue 4,2016.
|
Randomised control trial
|
- Changing operating room temperatures at the time of caesarean births reduces the rate of both neonatal and maternal hypothermia.
|
Görges M, Ansermino JM, Whyte SD. A retrospective audit to examine the effectiveness of preoperative warming on hypothermia in spine deformity surgery patients. Paediatric Anaesthesia. 2013 Nov;23(11):1054-61.
|
Evidence from a single site retrospective audit of spinal surgical paediatric patients |
- Preoperative warming in paediatric spinal patients significantly reduces time being hypothermic and potentially reduces the risk of perioperative complications.
|
Işler, A., Aydin, R., Güven, Ş. T., & Günay, S. (2014). Comparison of temporal artery to mercury and digital temperature measurement in pediatrics. International Emergency Nursing, 22(3), 165-168. doi:10.1016/j.ienj.2013.09.003
|
Evidence from a single site study.
|
- Evidence of measurement of temperature in paediatrics.
|
Leduc, D., & Woods, S. (2017). Position statement Temperature measurement in paediatrics.
|
Position statement
|
- The presence of a fever in children younger than three months of age triggers a thorough investigation into the source of the infection
|
Nemeth, M and Miller Clemens. Perioerpative Hypothermia in Children. International Journal of Environmental Research and Public Health. 2021, Volume 18.https://api.semanticscholar.org/CorpusID:236210212
|
Evidence from a review
|
- Describes the importance of perioperative warming in paediatrics.
|
Ralph, Nicholas. Preventing perioperative hypothermia is clinically feasible and cost effective. Journal of Perioperative Nursing: 2021Vol. 32 : Iss. 1 , Article 1. Available at: https://doi.org/10.26550/2209-1092.1051
|
Editorial |
- Describes the benefits of preventing perioperative hypothermia.
|
Ramjist JK, Sutthatarn P, Elliott C, Lee KS, Fecteau A. Introduction of a Warming Bundle to Reduce Hypothermia in Neonatal Surgical Patients. J Pediatr Surg. 2024 May;59(5):858-862.
|
Evidence from single site retrospective analysis.
|
- Using radiant warmer for neonates and hat decreased the proportion of hypothermic patient during and after surgery.
|
Zhang, MQ., Ying, PD., Wang, YJ. et al. Intraoperative hypothermia in the neonate population: risk factors, outcomes, and typical patterns. J Clin Monit Comput 37, 93–102 (2023).
|
Retrospective study from a single site
|
- Incidence of intraoperative neonatal hypothermia was 81.05%.
|
PG18 (A) Guideline for monitoring during anaesthesia
|
Anaesthesia Guideline
|
|
Please remember to read the
disclaimer.
The revision of this nursing guideline was coordinated by Tania Ramos, CNC, Nursing Research and approved by the Nursing Clinical Effectiveness Committee. Updated October 2024.