RCH Clinical Practice Guideline Paediatric Fractures
VFPMS Guideline: Forensic investigation of
fractures
A fracture is a complete or incomplete break
in the continuity of a bone.
Children’s bones fracture more easily than
adults’ bones. Fractures are common injuries sustained accidentally by active
children.
Fractures are also commonly detected in abused
infants and young children.
Physical examination alone can fail to detect
fractures in pre-verbal and relatively immobile infants. This means that
radiological investigations might be the only way to detect occult (hidden)
fractures in this age group.
Key points:
- Many children with fractures
have minimal or no external sign of injury. This means that the skin over
fracture sites can appear entirely normal.
- In childhood, most fractures
are caused by accidental falls and collisions.
- In infants, particularly pre-mobile
infants, fractures are more commonly attributed to abuse than to
accidents.
- No specific fracture location
or type is pathognomonic for abuse.
- Some fracture locations and
types of fracture (for example, classic metaphyseal lesion patterned
fractures at the ends of long bones and posteromedial rib fractures) are
more commonly attributed to inflicted trauma than to accidents.
- Fractures at different stages
of healing suggests that trauma occurred on different dates.
- Inflicted trauma (child abuse)
can result in multiple fractures affecting multiple bones and/or fractures
that appear to be at different stages of healing
- Dating of fractures is inexact.
Only an estimate can be made of the window of time in which bone injury
might have occurred.
Clinical Advice:
The following information should be obtained about the
presenting symptoms and signs. Ask about.
- Timing and detailed information about mechanism of
injury (for example, information about impacting surface and objects,
position of child when first observed after traumatic event)
- Circumstances surrounding the injury (Who was present?
Who heard or saw what? What was happening prior to the event and what
happened in the minutes to hours after?)
- Symptoms and signs of injury. Ask about deformity, signs
suggesting pain, alteration to limb function, swelling and other signs of
skin and soft tissue injury
The following information should be obtained about the past
medical history. Ask about.
- Medical conditions and treatment (particularly
endocrine disorders, renal and liver disease)
- Accidents (particularly past fractures and
dislocations)
- Medication
- Developmental milestones and current developmental
skills
The following information should be obtained about the family
history. Ask about.
- Consanguinity
- Inherited bone and connective tissue diseases / genetic
conditions
- 3 generation genogram regarding fractures and
dislocations
The following information should be obtained about the social
history. Ask about.
- Prior engagement with Child Protection and/or police.
Protective and Family Violence orders
- Child-care arrangements (and recent child carers’
contacts with the child)
- Violence in the home (safety) and disciplinary
practices
- Parental alcohol and drug use (past and recent)
- Parental mental illness and treatment
- Parenting experience, skills and capacity
Examination tips
- Standing back, observe
patient for possible bone deformity
- Thoroughly examine and
palpate the scalp, torso and limbs. Search for signs of swelling and tenderness
(a subjective sign)
- Observe gait. Observe the
movement, function and voluntary use of limbs
Investigations are unlikely to be required when
- The accident/ traumatic event involving an older child has
been witnessed by multiple observers (for example a child’s fall on an
outstretched hand while at school) and there are no concerns about child
abuse.
- There is a low probability of child abuse
(determination based on the totality of clinical findings).
- The age of the child and the fracture location and type
are strongly associated with accidental causes and not associated with
inflicted causes (for example, Colles fracture of the distal radius,
toddler fracture of the distal tibia, fracture of the clavicle in an
independently ambulant child)
Consider investigations when
- A fracture is
identified in a very young infant and birth trauma can be confidently excluded
- A fracture
(particularly an occult fracture) is identified in a pre-mobile (not yet
crawling or cruising) infant
- A fracture that has a
strong association with an inflicted mechanism is identified
- A fracture is
identified for which there is no apparent explanation
Investigations
Blood tests and
referral to specialists
|
First line investigations
|
- Full Blood Examination (FBE)
- Serum levels of calcium, phosphate and alkaline
phosphatase
- Liver Function Tests (LFTs)
- U&E and creatinine
- If child is <6months-old or in the presence
radiological evidence of osteopenia, consider 25OH vitamin D,
parathyroid level
- Consider consulting a paediatric radiologist
regarding possible radiological signs of bone dysplasia or metabolic
bone disease
|
|
Consider additional investigations and
referral to specialists based on clinical findings and results of
investigations
|
- Urinary calcium excretion (for example with a random
urinary calcium/creatinine ratio) when hypercalciuria is considered
- Septic work-up and inflammatory markers when
osteomyelitis is considered
- Copper and ceruloplasmin levels when Menkes’ disease
is considered
- Syphilis serology when syphilis is considered in the
presence of subperiosteal new bone formation or any other suggestive
clinical signs
- Consult an endocrine specialist in metabolic bone
disorders when considering possible bone dysplasias and metabolic bone
disorders
- Consult with a geneticist regarding inherited bone
dysplasias and consider genetic testing for Osteogenesis Imperfecta (OI)
and / or connective tissue disorders known to be associated with a
propensity to fracture
|
Radiological
investigations
The VFPMS supports the RANZCR October 2022 guideline for
imaging of suspected non-accidental injury[AS1] .
- In young children
(<2years-old) with a known fracture, consider investigations to search
for additional but occult fractures.
- In the presence of fractures
suggesting the application of significant force to the torso, consider
screening for abdominal injury.
- In selected cases (including a
young infant with a fracture) consider screening tests for possible head
injury.
Radiological Investigations
for occult fractures:
1. When bruising prompts investigations for
occult fractures
The VFPMS supports the RANZCR October 2022 guideline for imaging of suspected non-accidental injury
The VFPMS supports the Wood et al (2014) recommendations
regarding radiological investigations for occult fracture, as presented in the
following table. These recommendations were developed by a panel of US child
abuse experts’ consensus using a Delphi process.
|
I.
|
Skeletal survey is necessary in
children <24 months old with bruising if any of the
following features are present:
- History of confessed abuse
- History of bruising occurring during domestic violence
- Additional injuries on physical exam (e.g. burns,
whip marks)
- Patterned bruising
- >4 bruises NOT limited to bony prominences
- Ear, neck, torso, buttock, genital region, hands,
feet if there is no history of trauma
|
|
II.
|
Skeletal survey is also necessary in
children <12 months old with bruising in the following
locations:
- Cheeks, eye area, ear, neck
- Upper arms or legs (not over bony prominences)
- Hands, feet
- Torso, buttocks, genital region
- >1 bruise NOT limited to bony prominences
|
|
III.
|
Skeletal survey is also necessary in
children <9 months old with bruising in the following
locations:
- >1 bruise in ANY location
|
|
IV.
|
Skeletal survey is also necessary in
children <6 months old with bruising in the following
locations:
- Bony prominences (head T-shaped area, frontal scalp,
extremity bony prominences) EXCEPT if a single bruise and patient
presents with history of fall
|
|
These guidelines apply to children who do
not have a verifiable mechanism of accidental injury (i.e. MVC or fall in
public place), do not have underlying bleeding disorder such as haemophilia,
and who do not have a clear history of birth trauma that accounts for the
injury.
|
Wood JN et al. (2015)
Development of Hospital-Based Guidelines for Skeletal Survey in Young Children
With Bruises. Pediatrics. 135(2);e312-20.
2. When known fracture prompts investigations
for additional occult fractures
The VFPMS supports the
RANZCR October 2022 guideline for imaging of suspected non-accidental injury.
The VFPMS supports the Wood et al (2014) recommendations
regarding radiological investigations for occult fracture, given a fracture has
been identified, as presented in the following table. These recommendations
were developed by a US panel of experts using a Delphi methodology when only a
single skeletal survey was the most commonly used radiological investigation
for occult bone injury. The RANZCR guideline is preferred over the Wood
recommendations when advice is in conflict.
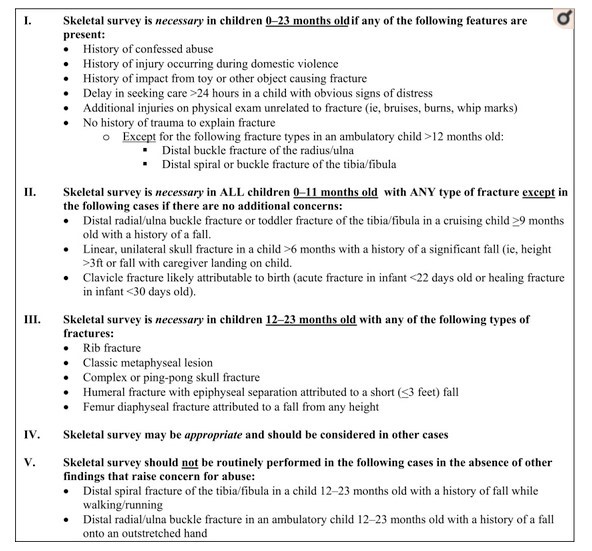
Wood JN et al. (2014)
Development Hospital-Based Guidelines for Skeletal Survey in Young Children
With Fractures. Pediatrics. 134(1);45-53.
Age of child
As discussed in the tables above, radiological
investigations for occult fractures are more often recommended in children
under the age of 2years.
When there is a strong suspicion of occult
fracture in older children (generally up to 5years of age) then consideration may
be given to performing a skeletal survey.
Useful resources and articles: